Abstract
Clear cell renal cell carcinoma (ccRCC) is the most common renal malignancy. However, the combined clinical and biological scores commonly used to predict the clinical outcome are imperfect and need improvement. The main goal of our study was to assess the effect of mtDNA genetics on the prognosis of ccRCC patients and to explore morphologic correlation. Mitochondrial DNA copy number (mtDNAcn) variation between tumor and paired matched healthy kidney tissue was assessed by real-time quantitative PCR and expressed as a ratio in 105 patients. According to this median ratio, the cohort was divided into two groups: “LOW” (n = 53) and “HIGH” (n = 52). Cancer-Specific Survival (CSS) and Disease-Free Survival were assessed in each group. The tumor samples were classified into two subtypes (Clear or Eosinophilic cells) according to the cytoplasmic morphology. CSS was significantly reduced in the “HIGH” than in the “LOW” group with respective 5-year survival rates: 78.7% (CI 95: 64.8–95.5) and 95.5% (CI 95 87.1–100.0) (Hazard Ratio: 7.4 (CI 95: 1.9–29.9, p = 0.027*) in multivariate analysis, including pathological classification, tumor size, International Society of Urological Pathology grade, lymphovascular invasion, dedifferentiated pattern, necrosis and adjuvant therapy. Next-generation sequencing of mtDNA was performed on 14 tumors and matched healthy kidney tissue. No hotspot mutation or redundant large deletion was found. None of the variants or large deletions identified had an impact on prognosis. MtDNAcn variation in tumor relative to normal kidney appears as an independent prognostic factor in ccRCC, which was also associated with eosinophilic morphology. MtDNA content could be considered an additional prognostic factor, in combination with other predictive parameters. Furthermore, these results underline the importance of the role of mitochondria in ccRCC and the need for further functional studies to understand the pathophysiological mechanisms better and consider therapies targeting mitochondrial metabolism.
Introduction
Clear cell renal cell carcinoma (ccRCC) is the most common renal cancer type (90%), with nearly 300,000 (2.6%) new cases yearly and higher incidence in developed countries [1, 2]. CcRCC is heterogeneous and characterized by clear or eosinophilic cells arranged in trabecular cords or nest architecture in a delicate stroma richly vascularized. The risk of recurrence post-nephrectomy for locally advanced kidney cancer is notably variable, with key factors including T stage, ISUP (International Society of Urological Pathology) grade, and the presence of necrosis or symptoms at diagnosis [3–5]. Various prognostic nomograms, such as UISS (University of California Los Angeles Integrated Staging System), ASSURE, and Leibovitch, have incorporated these clinical and pathological data [3, 6–10]. It is noteworthy that, as of now, no biological markers are employed in clinical practice to augment the prognostic precision of existing models.
As metabolic reprogramming is one of the hallmarks of cancer and mitochondria play a central role in metabolism, their role in carcinogenesis has been evaluated for years [11, 12]. CcRCC is characterized by a metabolic shift from mitochondrial oxidation to anaerobic glycolysis in the presence of oxygen, known as the Warburg effect [13–15], driven by the loss of function of the Von Hippel-Lindau gene (VHL) and the Hypoxia-inducible Factor (HIF) stabilization [16, 17].
In ccRCC, somatic variants in the nuclear genome accumulate according to the phylogenetic clone model, retaining a driver strain defect: the bi-allelic inactivation of VHL [18]. Other mutated genes are numerous and most often affect polybromo-1 (PBRM1), SET domain containing 2 (SETD2) or BRCA1-associated protein 1 (BAP1) genes [18–20], which are involved in methylation or chromatin compaction phenomena. Mitochondrial DNA (mtDNA) is a 16,569 bp circular double-stranded DNA molecule, maternally inherited. It encodes 13 polypeptides involved in oxidative phosphorylation (OXPHOS), and regulates reactive oxygen species (ROS) [21]. The accumulation of qualitative alterations and/or quantitative variation of mtDNA has been found to play a crucial role in carcinogenesis and metastasis, among other elements, by modulating cellular metabolism [11, 12]. Variations in mtDNA and their consequences on survival and disease progression are variable among cancers. In cancer subtypes of renal origin (chromophobe carcinoma) or non-renal origin (adrenocortical carcinoma or glioblastoma), high mtDNA copy number (mtDNAcn) is associated with better survival [22–24]. Conversely, a significant increase in mtDNAcn is associated with poorer prognosis in melanoma or breast carcinoma [22, 25]. In ccRCC, the impact of mtDNAcn on prognosis is conflicting. Some studies have shown that an increase in mtDNAcn relative to normal matched normal tissue is associated with a worse prognosis [22]. Still, other studies have suggested that a decrease in mtDNAcn compared to normal paired tissue and mitochondrial respiratory chain activity in vitro is associated with increased tumor growth, invasion capacity, and drug resistance mechanisms [26].
The first aim of this study was to assess the influence of mtDNA genetics (a.k.a mitochondrial copy number variation, deletions, and mutations) on the prognosis in patients with ccRCC and to explore histologic correlation. As an exploratory second aim, we looked at the impact of mtDNA depletion on cell proliferation in a ccRCC cell line.
Materials and methods
Population of the study
We retrospectively included 144 patients treated at Angers University Hospital from 2011 to 2019 for locally advanced ccRCC. Patients were registered in the UroCCR database (French Research Network for Kidney Cancer, NCT03294563, with the French data protection authority (CNIL) agreement DR-2013-206. Patients’ biological samples were stored in a biocollection of the Biological Resource Center (DC-2014-2224) in Angers Hospital. Written informed consent was obtained from all individuals with the approval of the research ethics committee of Angers University Hospital (authorisation number 2021-014). CcRCC diagnosis was established by an experienced pathologist. Metastatic patients at diagnosis, patients with other histological subtypes, patients who received chemotherapy, immunotherapy or targeted therapy before surgery, or who had less than 2 years of clinical follow-up were excluded. After partial or radical nephrectomy, fresh tumors and matched adjacent-healthy kidney tissue were snap frozen and long-term stored in liquid nitrogen (−196°C) at the biological resource centre (BRC) of Angers Hospital. One piece of the frozen tumoral sample was formalin-fixed and paraffin-embedded (FFPE) as a morphological control.
Disease-free survival (DFS) and Cancer-Specific Survival (CSS) were assessed using the date of recurrence, death, or the last clinical follow-up, respectively. Eight patients who did not die from ccRCC were excluded from CSS analysis. All clinical, pathological, and demographic data used for statistical analyses are available in Supplementary Table S1.
DNA extraction, mtDNA quantification and mtDNA sequencing
DNA extraction was performed using Qiamp DNA Mini kit (Qiagen, Hilden, Germany) according to manufacturer’s instructions and quantified by Nanodrop®2000 (Thermo Fischer Scientific, Waltham, Massachusetts, USA).
Mitochondrial DNA copy number (mtDNAcn) was assessed as previously described [27] by real time quantitative Polymerase Chain Reaction (Q-PCR). For each sample (tumor and healthy kidney tissues), the mtDNAcn was determined by the ratio of the mean copy number of two mitochondrial genes (MT-CO1 and MT-ND4) and two nuclear genes (B2M: beta2-microglobulin and GAPDH: glyceraldehyde 3-phosphate dehydrogenase). The real-time quantitative PCR (Q-PCR) was performed using the Chromo4 System (Biorad®, Hercules, CA, USA) in a 20 μL reaction volume containing ×1 IQ SYBR Green Supermix (Biorad®) and a final concentration of 0.5 μM of each gene-specific primer and 3 μL of template. The details of the primers are available in Supplementary Table S2.
For each patient, mtDNAcn variation between the tumor and adjacent normal tissue was expressed as a ratio (Tumor/Healthy Kidney: T/HK). Patients were then subdivided into two groups according to this ratio median: LOW mtDNAcn ratio (≤median) and HIGH mtDNAcn ratio (>median).
High-throughput mtDNA Next Generation Sequencing (NGS) was performed using Ion Torrent Proton, and the signal processing and base calling were done by our in-house bioinformatic pipeline on 14 tumor-healthy tissue pairs as previously described [27]. All somatic mutations in coding or non-coding mtDNA sequences were collected, and variants were classified as homoplasmic (>95% mtDNA) or heteroplasmic (<95%) according to their variant allele frequency. Large mtDNA rearrangements were searched using eKLIPse software [28].
Morphological and immunochemical analysis
FFPE morphological control was assessed blindly to genetic data. Cytoplasmic eosinophilia was rated microscopically as follows: 0: <5% eosinophilia, 1: 5%–20%, 3+: >90% and 2+: neither 1+ nor 3+ (Supplementary Figure S1). Scores 0 and 1+ were combined into the Clear Cells (CC) group, and scores 2+ and 3+ were encompassed in the Eosinophilic (EO) group. Because of intra-tumoral heterogeneity, ISUP corrected (ISUPc) grade [29] was assessed and assigned to each frozen sample (Supplementary Table S1).
Immunohistochemistry was performed on whole slide sections using an automated immunochemistry system (Leica Bond III, Wetzlar, Germany) with TOMM20 antibody (Translocase of the outer mitochondrial membrane complex subunit 20, Abcam, Cambridge, UK, ab186735, clone EPR15581-54, 1:1000). TOMM20 is an outer mitochondrial membrane protein. Its expression would support that eosinophilic morphology is related to mitochondria rather than other organelles.
MtDNA depletion in 786-O cell line and cell imaging
786-O CcRCC cell line (ATCC number CRL-1932, Boulogne Billancourt, France) was gradually devoided of mtDNA content using Ethidium Bromide (BET) (Sigma-Aldrich Saint Louis, Missouri, USA) at 200 ng/mL for 7 days. 786-O cells were maintained in Dulbecco’s modified Eagle’s medium (DMEM) with 4.5 g/L glucose (Pan Biotech, Bernolsheim, France), supplemented with 10% of Fœtal Bovine Serum (FBS) (Good Pan, Pan Biotech), 1% of glutamine (Dominique Dutscher, Bernolsheim, France), 1% of uridine (Pan Biotech), 1% of pyruvate (ThermoFisher Scientific) and incubated at 37.5°C under a 5% CO2 atmosphere. The culture medium was changed every day.
To standardize the cell culture conditions, 786-O-WT wild type (not depleted) and 786-O-D (mtDNA depleted) cells were cultured under the same supplied medium conditions. Briefly, cells were plated in quadruplets in one plate with three biological replicates. One well was trypsinized (Pan Biotech) and extracted on day 4 to assess the level of mtDNAcn as described above. All remaining wells were trypsinized and extracted on day eight. Cell proliferation was evaluated using live cell imaging (IncuCyte ZOOM system, Sartorius, Gottingen, Germany), taking images every 2 h, and estimated as the ratio between the well’s confluence (%) calculated during 8 days (192 h) reported to the cellular confluence at day 0 by using the Basic Analyzer segmentation mask of the IncuCyte ZOOM software 2015A.
Statistical analyses
Quantitative data were expressed with median or mean and interquartile range (median or mean; [IQR]). Qualitative data are given as percentages. Survival data are provided with the hazard ratio (HR) and 95% confidence interval (CI95%). Chi-2 test (qualitative data), Mann-Whitney test (quantitative data), log-rank test, and Kaplan-Meier curve (survival data) were performed on SAS JMP 10 software (SAS Institute Inc, NC, USA) or GraphPad Prism 9 (San Diego, USA). When needed, Benjamini and Hochberg’s corrections were performed. P value < 0.05 was considered significant. Multivariate analysis was performed using the Cox model.
Results
Constitution of the cohort
One hundred and five patients constituted the final cohort of our study. The inclusion process is summarized in Figure 1.
FIGURE 1
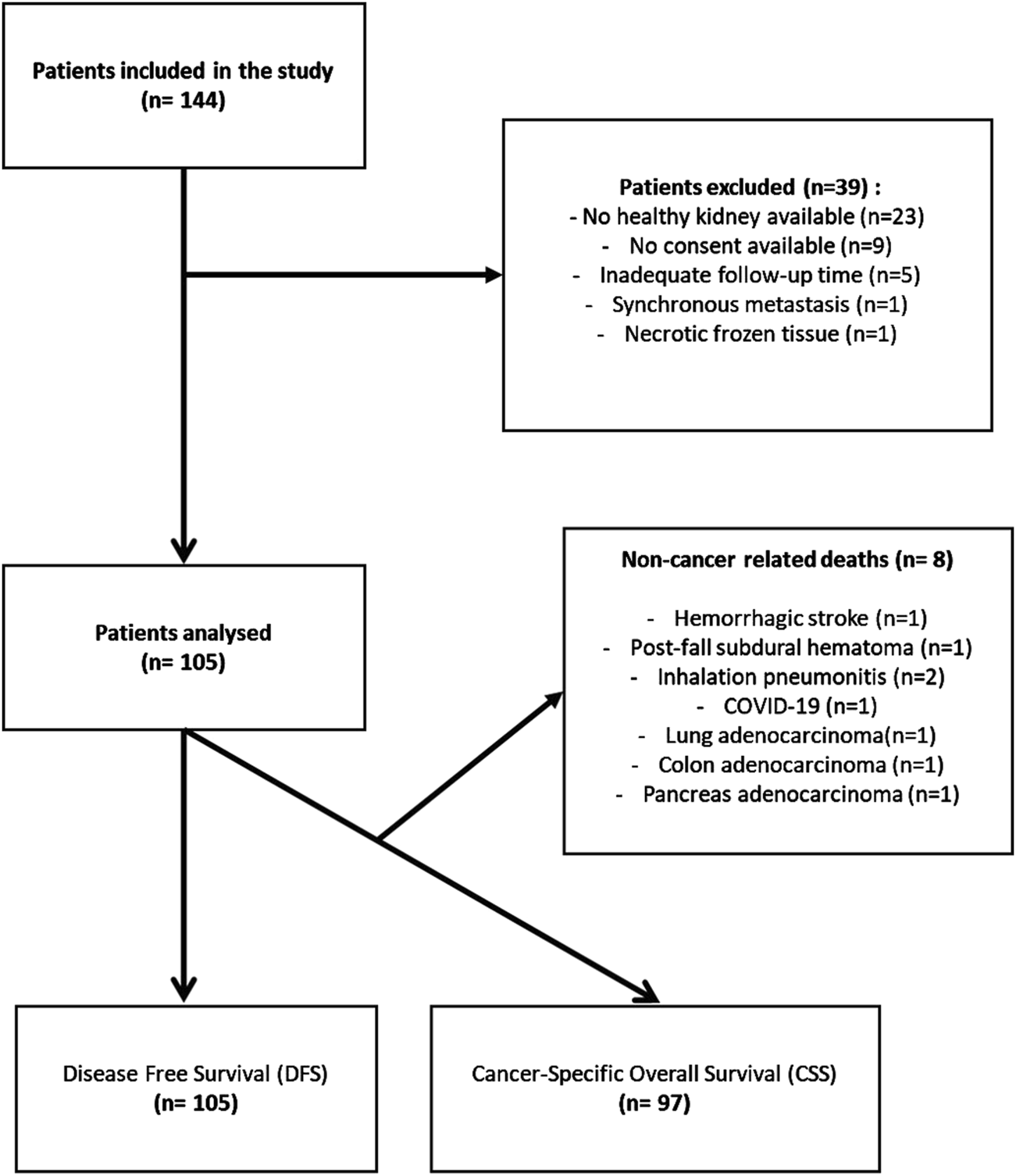
Flow Chart representing the patient’s inclusion process and group analyses.
In the overall cohort, the median age was 64 years [56.0–73.0], and the sex ratio (Male/Female) was 1.7:1. The median follow-up was 53 months [36.0–78.0]. Demographic, histologic, clinical and molecular data are summarized in Table 1. Four patients received adjuvant therapy. One patient received Vascular Endothelial Growth Factor (VEGF) inhibitors and an immune checkpoint inhibitor, one patient received VEGF inhibitors only, and two patients received immune checkpoint inhibitors.
TABLE 1
| LOW (n = 53) | HIGH (n= 52) | p-value | |
|---|---|---|---|
| Age at diagnosis mean (standard deviation) | 63.1 (±11.5) | 64.6 (±12.5) | 0.51 |
| >60 years old n (%) | 33 (62%) | 33 (63%) | 0.89 |
| <60 years old n (%) | 20 (38%) | 19 (37%) | |
| Sex | 0.59 | ||
| Men n (%) | 32 (60%) | 34 (65%) | |
| Women n (%) | 21 (40%) | 18 (35%) | |
| ISUP Grade | 0.06 | ||
| 1–2 n (%) | 19 (36%) | 10 (19%) | |
| 3–4 n (%) | 34 (64%) | 42 (81%) | |
| ISUP grade corrected | 0.011a | ||
| 1–2 n (%) | 48 (91%) | 37 (71%) | |
| 3–4 n (%) | 5 (9.4%) | 15 (29%) | |
| Tumor Size (standard deviation) | 6.17 (±2.60) | 6.39 (±2.40) | 0.64 |
| pT | 0.20 | ||
| 1–2 n (%) | 29 (55%) | 22 (42%) | |
| 3–4 n (%) | 24 (45%) | 30 (58%) | |
| pN | 0.31 | ||
| Nx-N0 n (%) | 53 (100%) | 51 (98%) | |
| N1-N2 n (%) | 0 (0%) | 1 (1.9%) | |
| Necrosis n (%) | 18 (34%) | 20 (38%) | 0.63 |
| Lymphovascular invasion n (%) | 22 (42%) | 19 (37%) | 0.60 |
| Sarcomatoid or Rhabdoid pattern n (%) | 2 (3.8%) | 3 (5.8%) | 0.63 |
| Positive surgical margin | 0 (0%) | 1 (1.9%) | 0.31 |
| Surgical specimen | 0.13 | ||
| Nephrectomy | 41 (77%) | 46 (88%) | |
| Tumorectomy | 12 (23%) | 6 (12%) | |
| UISS group, n(%) | 0.030* | ||
| Intermediate | 35 (66%) | 38 (73%) | |
| High | 6 (11%) | 11 (21%) | |
| Low | 12 (23%) | 3 (5.8%) | |
| SSIGN group, n(%) | 0.28 | ||
| Intermediate | 26 (49%) | 31 (60%) | |
| Low | 23 (43%) | 15 (29%) | |
| High | 4 (7.5%) | 6 (12%) | |
| GRANT group, n(%) | 0.17 | ||
| Favorable | 50 (94%) | 45 (87%) | |
| Unfavorable | 3 (5.7%) | 7 (13%) | |
| Morphology n(%) | 0.005* | ||
| Clear | 36 (68%) | 21 (40%) | |
| Eosinophilic | 17 (32%) | 31 (60%) | |
| Relapse, n(%) | 17 (32%) | 23 (44%) | 0.19 |
| Adjuvant therapy, n(%) | 3 (5.7%) | 1 (1.9%) | 0.31 |
| Disease-Free Survival (months, mean) | 45.6 (±29.5) | 40.5 (±32.7) | 0.49 |
| Specific Overall Survival (months, mean)a | 62.8 (±34.0) | 56.4 (±30.3) | 0.44 |
| Ratio mtDNAcn (tumor/healthy kidney), mean (standard deviation) | 0.21 (±0.0705) | 0.81 (±0.950) | <0.0001* |
Clinicopathological and molecular characteristics of the study population according to HIGH and LOW groups.
Overall survival analysis was performed for 97 patients. ISUP: International Society of Urological Pathology, pT: pathological Tumor status, pN: pathological Node status, UISS: UCLA Integrated Staging System, SSIGN: Stage Size, ISUP Grade, Necrosis, GRANT (Grade, Age, Node, Tumor). *Means significant difference.
Clinicopathological features and mtDNAcn quantification
In the overall cohort, mtDNAcn was significantly higher in healthy tissue than in tumor tissue, ranging from 52 to 1070 copies (mean:162; [118–256]) in tumor tissue (T) and from 79 to 1920 copies (mean: 569; [368–734]) in the healthy kidney (HK) tissue (p < 0.0001*), leading to a mtDNAcn ratio T/HK ranging from 0.08 to 6.24 [0.22–0.49]. The mean mtDNAcn in healthy tissue was not statistically different in patients who had renal failure (n = 5, p = 0.21). The cohort was then divided into two groups, HIGH and LOW, according to the median of this ratio. All the results reported hereafter concern both groups: the HIGH group corresponding to the less mtDNA-depleted tumors and the LOW group for the most mtDNA-depleted ones.
The mean mtDNAcn ratio T/HK was significantly higher in the HIGH group than in the LOW group, respectively 0.81 [0.41–1.23] vs. 0.21 [0.15–0.26] (p < 0.0001*). Both ISUP grade corrected 3-4 and eosinophilic morphology were more frequent in the HIGH group than in the LOW group (p = 0.011* and p = 0.005* respectively). The LOW group comprised more patients of low risk according to the UISS classification (p = 0.030*). No difference was seen in SSIGN or GRANT classification groups or in other classical clinical features (Table 1).
Increased mtDNAcn in ccRCC patients is associated with worse overall survival
Cancer Specfic Survival related to ccRCC-death was significantly worse in the HIGH than in the LOW group, with respective 5-year survival rates: 78.7% (CI 95: 64.8–95.5) and 95.5% (CI 95: 87.1–100.0) (Hazard Ratio HR: 7.4 (CI95: 1.9–29.9, p = 0.027*) (Figure 2A). In univariate analysis of CSS, tumor size, ISUPc grade, lymphovascular invasion, and mtDNAcn ratio were significantly associated with a worse prognosis. Only the mtDNAcn ratio was associated with a worse prognosis in multivariate analysis (p = 0.008*) (Table 2). There was no difference in DFS between the two groups (p = 0.17) (Figure 2B). Deaths related to ccRCC were significantly more prevalent in the HIGH group than in the LOW group (p = 0.021*, Odds Ratios (OR): 7.8 (CI95: 0.92–66.3). No difference was found regarding relapses (p = 0.56).
FIGURE 2
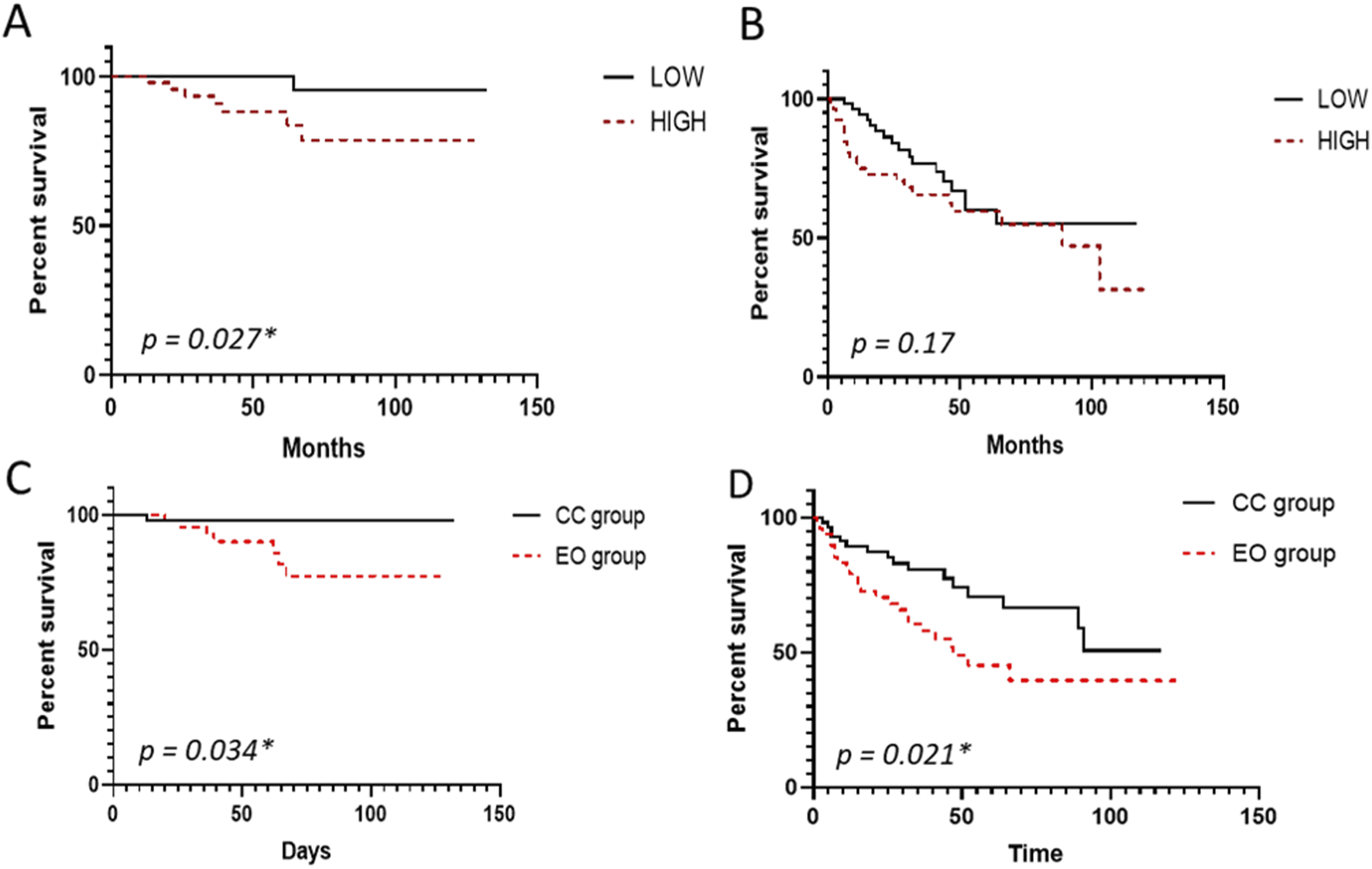
Survival curves according to mtDNA copy number and morphology. Survival Kaplan Meier curve representing (A) Cancer-specific survival and (B) Disease-free Survival in the HIGH and LOW groups, (C) Cancer-specific survival, and (D) Disease-free Survival in the Eosinophilic (EO) and Clear Cell (CC) groups.
TABLE 2
| Specific overall survival analyses. Cox model; proportional hazards adjustment | ||||
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| HR (CI 95%) | p Value | HR (CI 95%) | p Value | |
| HIGH vs. LOW ratio Groups (mtDNAcnT/HK) | 4,79 (1.20; 9.22) | 0.020* | 13.96 (1.84; 313.94) | 0.008* |
| pT (3–4 vs. 1–2) | 7.39 (1.75; 31.32) | 0.007* | 0.64 (0.03; 14.25) | 0.77 |
| pN (1–2 vs. 0-X) | 0.36 (1.29e-24–1026) | 0.80 | 3.86e-11 (0; 19.03) | 0.29 |
| ISUP grade (3–4 vs. 1–2) | 3.59 (0.66; 19.40) | 0.13 | 3.31e+08 (0.30; 1.06e+62) | 0.21 |
| ISUPc grade (3–4 vs. 1–2) | 6.86 (1.2; 39.30) | 0.030* | 0.87 (0.16; 5.02) | 0.87 |
| Necrosis (presence vs. absence) | 2.45 (0.60–10.06) | 0.21 | 1.45 (0.31; 8.21) | 0.63 |
| Lymphovascular invasion (presence vs. absence) | 4.66 (1.12; 19.42) | 0.034* | 12.65 (0.98; 501.20) | 0.05 |
| Sarcomatoid or rhabdoid pattern (presence vs. absence) | 3.10 (0.17; 56.58) | 0.44 | 3.40 (0.05; 111.77) | 0.50 |
| Adjuvant therapy (yes/no) | 1.65 (0.18; 15,41) | 0.86 | 3.11 (0.05; 95.35) | 0.52 |
| Eosinophilic (EO) vs. Clear (CC) Group | 6.96 (1.74–27.84) | 0.034* | 1.18 (0.16–11.52) | 0.87 |
Univariate and multivariate statistical analyses of specific overall survival by the Cox model.
ISUP: International Society of Urological Pathology, pT: pathological Tumor status, pN: pathological Node status. *Means significant difference.
Eosinophilic features were associated with high mtDNAcn and worse prognosis
Cytoplasmic eosinophilia was rated in all tumors: 54% (n = 57) were classified as CC and 46% (n = 48) as EO. The EO group was significantly associated with the “HIGH” group (p = 0.005*). ISUP grade 3–4, and ISUP grade corrected 3-4 and necrosis were more prevalent in the EO group than in the CC group (p = 0.012*, p < 0.001*, p = 0.022* respectively). The mean tumor size was slightly higher in the EO group than in the CC group (6.8 cm [5–8.5] vs. 5.8 [4–7], p = 0.039*). The mtDNAcn was significantly higher in the EO (mean: 235; [163–343]) than in the CC group (mean: 125 [101–168]) (p < 0.0001*). All clinicopathological data related to the EO vs. the CC group are summarized in Supplementary Table S3.
Deaths due to ccRCC were significantly more prevalent in the EO group than in the CC group, with Odds Ratios (OR) of 8.6 (CI95: 1–72.6; p = 0.021*). No difference was seen in relapses (p = 0.05).
In univariate analysis, the 5-year CSS rate in the EO group was significantly reduced compared to the CC group, respectively 77.3% (CI95: [63.2–94.6]) and 98% (CI95: [94.1–100]) (p = 0.034*) (Figure 2C). The DFS was significantly shorter in the EO group than in the CC group, with 5-year survival rates of 39.6% (CI95: [25.5–61.5] for EO compared to 50.7% CI95: [32.4–79.3] for the CC group (p = 0.021*) (Figure 2D). However, it was not an independent prognostic factor in multivariate analysis for overall specific cancer survival (p = 0.87).
Immunohistochemistry showed that TOMM20 was diffusely expressed in EO compared to the CC group (Figure 3), showing that eosinophilic morphology is related to mitochondria and supporting the molecular data showing that EO cells were enriched in mtDNA.
FIGURE 3
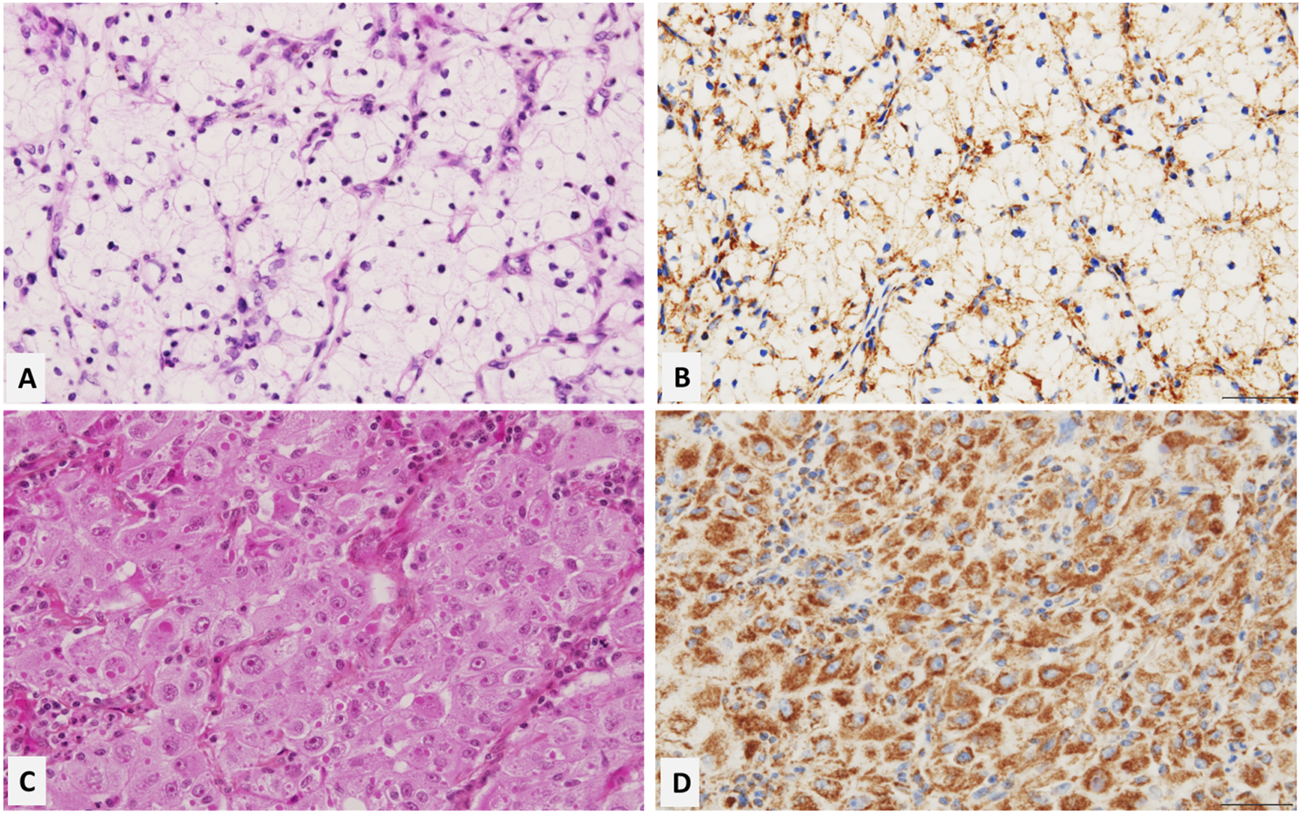
Representative microscopic images of clear and eosinophilic cell features of ccRCC (Hematoxylin, Eosin, Saffron staining, and TOMM20 antibody staining (1/1000) x 100). The clear cell feature of ccRCC shows a weak and submembranous positivity for TOMM20 (A,B). The Eosinophilic feature of ccRCC shows strong and diffuse cytoplasmic positivity for TOMM20 (C,D). This data supports the enrichment of mitochondria in the eosinophilic regions of ccRCC.
CcRCC carries mtDNA variants without a mutation hotspot
High-throughput mtDNA NGS was performed on fourteen healthy kidneys and tumor pairs samples. It identified a limited number of somatic mutations in each tumor (1; [1–3.5]). The 39 somatic mutations identified appeared randomly distributed along the mitochondrial genome, regardless of interspecies conservation (Supplementary Table S4). Thirteen mutations were located in non-coding genes (D-loop, ribosomal or transfer RNAs) and 26 in coding genes (Complex I, III, IV, V). No mutational hotspot was identified. Heteroplasmy load was highly variable, ranging from 9.8% to almost homoplasmic variants (88%; [56.75–100]). The number of somatic mutations was not significantly different in the HIGH than in the LOW groups (p = 0.13). eKLIPse software [28] did not reveal the accumulation of large-scale mtDNA deletions in tumors (p = 0.71) (Supplementary Figure S2).
No statistical difference was found comparing the number of somatic mutations and the EO/CC group (p = 0.44). There was no statistical difference in the kind of somatic mutations between CC and EO groups (heteroplasmic variant: p = 0.61, non-coding variant: p = 0.74). There was no association between mtDNAcn and the number of somatic mutations (p = 0.21).
Depletion of mtDNAcn inhibits the proliferation of 786-0 cells in vitro
After 4 and 7 days of EB (Ethidium Bromide) exposure, the mtDNAcn of 786-O-D cells was reduced by 88% and 95% compared to untreated 786-O-D cells (Figure 4A). In this in vitro assay, mtDNA depletion was associated with a reduction in cell proliferation from day 4. After 7 days of treatment, the 786-O-D growth proliferation rate was 1.8 times slower than untreated cells (p = 0.0005*) (Figure 4B).
FIGURE 4
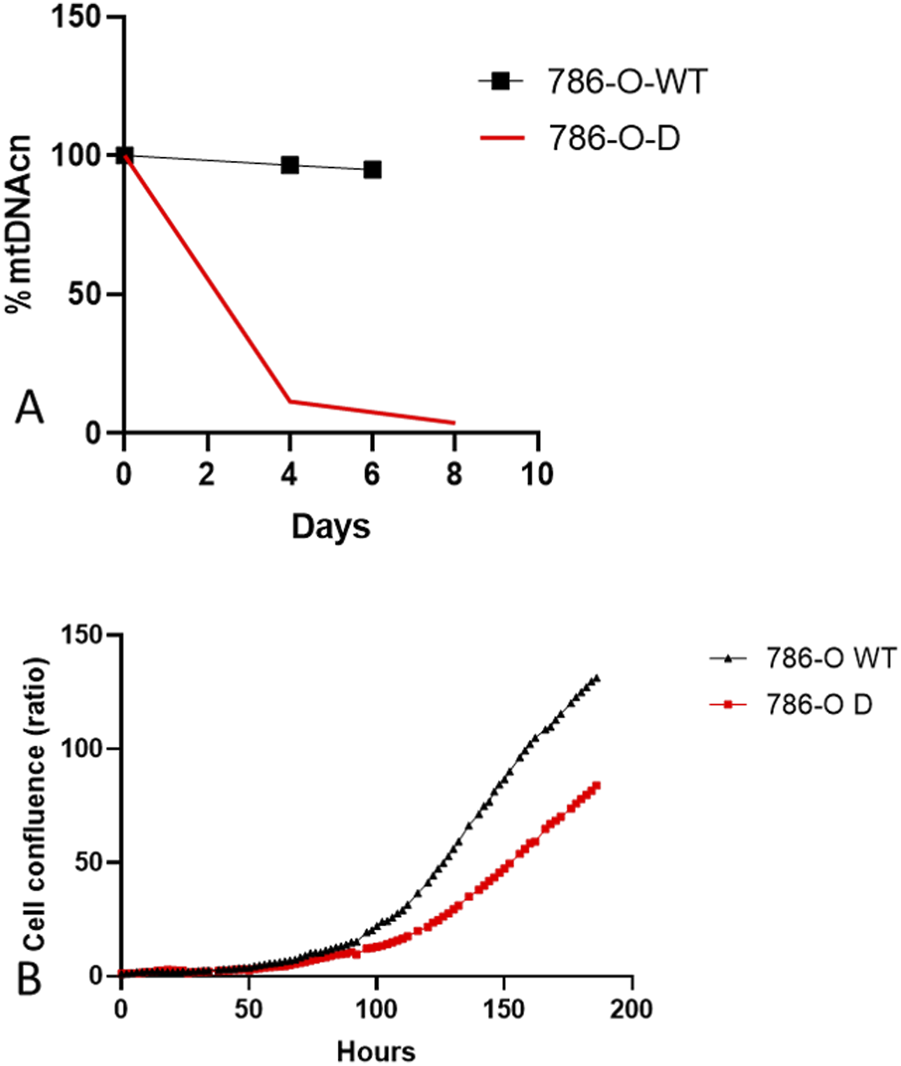
Normalized mtDNAcn and cell proliferation curves according to culture condition. (A) mtDNAcn evolution during culture in non-depletion conditions (786-O-WT) and depletion conditions (786-O-D) (B) Cell proliferation curves of 786-O-WT cells and 786-O-D were normalised at time 0.
Discussion
Mitochondria play a major role in multiple cellular functions, such as energy production, formation of reactive oxygen species [30, 31], and initiation of apoptosis [30, 32]. Mitochondrial dysfunctions are involved in tumorigenesis [33] through mechanisms of epithelial-mesenchymal transition [34] and metabolic changes (i.e., Warburg Effect) [13–15].
MtDNAcn variations during carcinogenesis are highly dependent on cancer subtypes [22–24, 35]. As previously described [22, 26], we observed that most ccRCCs showed an overall mtDNA depletion compared to the normal kidney. This finding is probably due to the loss of function of the VHL complex secondary to a biallelic inactivation of VHL [35, 36], which is present in more than 90% of ccRCCs. Indeed, VHL loss of function induces an abnormal activation of HIF, responsible for ccRCC’s distinctive metabolic reprogramming [36–38], the “Warburg effect” [16, 17], which promotes the shift of glucose use toward the lactate pathway instead of Oxidative Phosphorylation (OXPHOS) [13, 15]. In addition, through the inhibition of carnitine palmitoyltransferase 1A (CPT1A), HIF is responsible for reducing fatty acid transport into the mitochondria and compels the storage of fatty acids as lipid droplets in the cytoplasm [39]. Those mechanisms may partially explain why ccRCCs are naturally depleted in mitochondria, displaying minimal respiratory capacity [40] and harbouring a clear cell appearance [39]. In this context, as tumor cells appear to depend little on mitochondria (OXPHOS) for their metabolism, they may downregulate the level of mtDNAcn.
The effects of mtDNA depletion in in vitro models depend on the cell line origin and types of cancer. In breast cancer cell lines, for example, the mtDNAcn reduction slows down the cell proliferation rate and diminishes the tumorigenic phenotype [41, 42]. In contrast, glioblastoma cell lines maintain a tumorigenic phenotype through a low mtDNAcn as a result of a hypermethylation process as previously shown [43]. In vitro, we showed that mtDNA depletion decreases cell proliferation in the 786-O cell line, which is derived from a primary renal clear cell carcinoma, after being treated with BET. These results support our clinical data, suggesting that a lower mtDNAcn in the tumor is associated with a better prognosis in ccRCC, similar to breast cancer [25]. The opposite data were observed in chromophobe renal cell carcinoma or glioblastoma in young subjects under 40 years old, where an increase of mtDNAcn was associated with better prognosis and survival [22–26]. One limitation is that our in vitro study was designed to be exploratory and basic. It could be worthwhile to complete it with an additional essay exploring glucose or glutamine metabolites, for example.
We showed that the tumor mtDNAcn relative to that of healthy tissue was an independent prognostic factor in ccRCC patients. Indeed, the HIGH group ratio was associated with worse overall survival, with a 5-year survival rate of 78.7% compared to 95.5% in the LOW group.
Since 2021, pembrolizumab has exhibited its efficiency in reducing the likelihood of recurrence and mortality following nephrectomy for locally advanced kidney cancer [44, 45]. Despite its positive impact, this treatment induces many side effects, underscoring the importance of identifying patients at the highest risk of recurrence for optimal use in the years ahead. In our cohort, very few patients received adjuvant therapy such as targeted therapy (VEGF inhibitors) or an immune checkpoint inhibitor. The effect of adjuvant treatment did not influence our data. In the same way, there was no statistical difference in mtDNAcn in renal failure patients (n = 5) compared to others, so we believe that despite the morphologic control of frozen healthy renal tissue, it did not cause a bias.
Our results show that, within mitochondrial genetics, mtDNA copy number variation appears to play a more critical role in the physiopathology of ccRCC than the accumulation of somatic mutations. In our cohort, as previously described in renal cancer [11, 35, 46], few mtDNA somatic mutations were identified, mainly carrying low interspecies conservation scores and with a low to moderate impact on mitochondrial function, suggesting a transient rather than a driving role of those variants. However, NGS was performed on a small cohort, which may have limited the detection of certain anomalies due to a lack of power.
CcRCCs are heterogeneous tumors that can display clear or eosinophilic cytoplasm features in the same tumor. As explained above, the clear cell appearance of ccRCC is likely due to multiple mechanisms related to VHL inactivation. Moreover, ultrastructural and immunohistochemical studies have shown a higher number of mitochondria in eosinophilic ccRCC than in its clear cell counterpart [47–50]. Interestingly studies of intratumoral heterogeneity showed that the eosinophilic components of ccRCC are associated with poor prognosis outcomes [51, 52] compared to the clear cell components despite a common genetic background with VHL inactivation [18, 53]. In our study, although the diagnosis of ccRCC was done by an experienced pathologist who ruled out differential diagnosis bearing clear cell morphology, we did not sequence the VHL gene, which remains a limitation. This limitation is somewhat limited because VHL inactivation is present in almost all ccRCC. Indeed recent advances have identified new entities in renal carcinoma with clear cell morphology and VHL wild type phenotype such as TFE3-rearranged RCC, ELOC (formely TCEB1)-mutated RCC or clear cell renal papillary tumor [54–59].
Our data showed that eosinophilic morphology is associated with increased mtDNAcn and worse DFS and CSS. A recent study [52] has demonstrated the value of distinguishing ccRCCs’ clear cells from eosinophilic cells for the prognostic and therapeutic strategy. Indeed, eosinophilic ccRCCs, due to an abundant lymphocytic inflammatory infiltrate, are good responders to immunotherapy, whereas clear cells ccRCC, characterised by an abundant vascular stroma, have a higher sensitivity to targeted therapy [52]. Nilsson et al. [51] performed RNA sequencing on eosinophilic and clear cell RCC. They showed an overexpression in the eosinophilic component of the DNA polymerase subunit gamma (POLG) encoding for the POLG catalytic subunit, solely responsible for the mtDNA replication. The POLG induction may explain the increase of mtDNAcn in this contingent even though we currently do not know the mechanism responsible for POLG overexpression. Hence, the accumulation of mtDNAcn in eosinophilic areas is more likely due to an increase in mitochondrial biogenesis rather than a defect in the mitophagy process. Interestingly, in this study, the TFAM gene (Transcription Factor A, Mitochondrial) was downregulated, which could be surprising considering its function as an mtDNA transcription factor. However, TFAM is also identified as the significant mtDNA packaging protein, constituting the core component of the mitochondrial nucleoid [60, 61]. Hence, an increased TFAM expression results in stronger mtDNA compaction, making it less permissive to replication and mitochondrial genome accessibility [62]. As a result, TFAM underexpression enables replication consistent with the mtDNAcn increase.
It is important to better understand why and how the increase in mtDNAcn could benefit to ccRCC since it is naturally deprived (see above). One hypothesis is the metabolism of glutamine particularly because this one is favoured by the metabolic acidosis due to the Warburg effect [63, 64]. Glutamine is a non-essential amino acid provided by the diet and synthesised endogenously. Glutamine is further metabolised into glutamate supporting the biosynthesis of nucleotides and amino acids and the energy metabolism throughout the Tricarboxylic Acid Cycle (TCA), the OXPHOS via the production of mitochondrial citrate, and fatty acid beta-oxidation [32, 65, 66]. Glutamine would act as a proper energy substrate in this context while the glycolysis and beta-oxidation pathways are reduced [37, 65]. An increase in the number of mitochondria could be associated with an increase in glutaminolysis metabolism, providing the energy and nucleotide substrates necessary for tumor cell proliferation. Evidence supporting this hypothesis relies on the increased isocitrate dehydrogenase IDH1 gene expression in eosinophilic cells [51]. Hakimi et al [38] reported that tumor progression and metastasis were associated with increased metabolites in the glutathione pathway. Yet, glutathione is a tripeptide made of glutamate, cysteine, and glycine. Moreover, through the formation of glutathione and glutamate, glutamine enables tumor cells to resist to ROS overproduction and anoikis via autophagy phenomena [65, 67] and promotes the formation of metastases [65]. Moreover, it has recently been shown that the Solute Carrier Family 1 Member 5 (SLC1A5) transporter [68], which allows the entry of glutamine into the mitochondria, had an oncogenic role since its in vitro inactivation was associated with a reduction of tumor growth [68]. Further experiments should be done to investigate the glutamine pathway and metabolites in clear and eosinophilic cells in ccRCC. This hypothesis is supported by several in vitro and phase 1-2 studies performed in kidney cancer (papillary or clear cells). These studies showed that glutaminase inhibitors decrease cell growth proliferation and tumor size and potentiate the effects of targeted therapies, especially immunotherapies [69, 70]. Glutamine inhibitors act dually by inhibiting cell proliferation intrinsically (downstream signalling pathways) and by restoring the activation of effector T cells by increasing the availability of cytoplasmic glutamine. As we have seen above, eosinophilic cells are enriched in lymphocytic inflammatory infiltrate and mitochondria, so we would expect immunotherapies combined with glutaminase inhibitors to be beneficial in eosinophilic rather than clear cells ccRCC in future clinical trials.
Conclusion
In conclusion, high mtDNAcn in tumors compared to healthy kidneys is an independent factor of poor prognosis in ccRCC and is associated with an eosinophilic morphology which highlights the significance of identifying this pattern on pathological examination. The benefit of mtDNAcn increase for the tumor cell could be mediated through the glutamine metabolic pathway. If confirmed, this hypothesis may provide a new perspective on the pathological diagnosis and therapy of ccRCC, especially concerning the synergistic combination of immunotherapy and glutaminase inhibitors.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by comité d’éthique CHU Angers France. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Ethical approval was not required for the studies on animals in accordance with the local legislation and institutional requirements because only commercially available established cell lines were used.
Author contributions
SB and M-CC performed the pathology part. NB, CR, and VL encompassed the clinical data. OB supplied samples from the Biological Centre, SB and JR conducted the experiments on cell lines. SB and CB performed statistical analyses. All authors contributed to the writting of the manuscript and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by grants from the University and Hospital of Angers and the French League Against Cancer [49].
Acknowledgments
Thanks to Bové Leo for his technical support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.por-journal.com/articles/10.3389/pore.2025.1612172/full#supplementary-material
SUPPLEMENTARY TABLE S1Clinical, pathological, and demographic data used for statistical analyses. ISUP: International Society of Urological Pathology, pT: pathological Tumor status, pN: pathological Node status, UISS: UCLA Integrated Staging System, SSIGN: Stage Size, ISUP Grade, Necrosis, GRANT (Grade, Age, Node, Tumor).
SUPPLEMENTARY TABLE S2Primers used for mitochondrial DNA quantitative polymerase chain reaction.
SUPPLEMENTARY TABLE S3Clinical, pathological, and demographic data of Eosinophilic (EO) vs Clear (CC) groups. ISUP: International Society of Urological Pathology, pT: pathological Tumor status, pN: pathological Node status.
SUPPLEMENTARY TABLE S4Nature and location of identified mtDNA variants.
SUPPLEMENTARY FIGURE S1ccRCC’s grading system of eosinophilic features on Hematoxylin-eosin and saffron staining (X400): (A) 0, (B) 1+, (C) 2+, (D) 3+. (A) and (B) were merged into the Clear Cell group (CC group) and (C) and (D) into the eosinophilic group (EO group).
SUPPLEMENTARY FIGURE S2CIRCOS generated by eKLIPse software representing large scale mtDNA deletions observed in each patient.
Glossary
- 786-O-D
786-O mtDNA depleted
- 786-O-WT
786-O wild type
- B2M
beta2-microglobulin
- BAP1
BRCA1-associated protein 1
- BCR
Biological Resource Centre
- BET
Ethidium Bromide
- CC
Clear Cell
- CcRCC
Clear Cell Renal Cell Carcinoma
- CPT1A
carnitine palmitoyltransferase 1A
- CSS
Cancer-Specific Survival
- DFS
Disease-Free Survival
- DMEM
Dulbecco’s modified Eagle’s medium
- EO
Eosinophilic
- FBS
Fetal Bovine Serum
- FFPE
formalin-fixed and paraffin-embedded
- GAPDH
glyceraldehyde 3-phosphate dehydrogenase
- HIF
Hypoxia Inducible Factor
- IDH1
isocitrate dehydrogenase 1
- ISUP
International Society of Urological Pathology
- ISUPc
International Society of Urological Pathology Corrected
- MtDNA NGS
Mitochondrial DNA Next Generation Sequencing
- MtDNA
Mitochondrial genome
- MtDNAcn
Mitochondrial DNA copy number
- MT-ND1
Mitochondrially Encoded NADH: Ubiquinone Oxidoreductase Core Subunit 1
- NGS
Next Generation Sequencing
- OS
Overall Survival
- OXPHOS
oxidative phosphorylation
- PBRM1
polybromo-1
- POLG
polymerase subunit gamma
- Q PCR
Quantitative Polymerase Chain Reaction
- ROS
reactive oxygen species
- SCLA1A5
Solute Carrier Family 1 Member 5
- SETD2
SET domain containing 2
- T/HK
Tumor/Healthy Kidney ratio
- TCA
tricarboxylic acid cycle
- TFAM
Transcription Factor A, Mitochondrial
- TOMM20
Translocase of the outer mitochondrial membrane complex subunit 20
- UISS
University of California Los Angeles Integrated Staging System
- UroCCR
French Kidney Cancer Research Network
- VEGF
Vascular Endothelial Growth Factor
- VHL
Von Hippel Lindau
- VLDL-R
low-density lipoprotein receptor
References
1.
Ljungberg B Campbell SC Choi HY Cho HY Jacqmin D Lee JE et al The epidemiology of renal cell carcinoma. Eur Urol (2011) 60(4):615–21. 10.1016/j.eururo.2011.06.049
2.
Ferlay J Colombet M Soerjomataram I Dyba T Randi G Bettio M et al Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer (2018) 103:356–87. 10.1016/j.ejca.2018.07.005
3.
Patard JJ Kim HL Lam JS Dorey FJ Pantuck AJ Zisman A et al Use of the University of California Los Angeles integrated staging system to predict survival in renal cell carcinoma: an international multicenter study. J Clin Oncol (2004) 22(16):3316–22. 10.1200/JCO.2004.09.104
4.
Delahunt B Eble JN Samaratunga H Thunders M Yaxley JW Egevad L . Staging of renal cell carcinoma: current progress and potential advances. Pathology (2021) 53(1):120–8. 10.1016/j.pathol.2020.08.007
5.
Kuthi L Jenei A Hajdu A Németh I Varga Z Bajory Z et al Prognostic factors for renal cell carcinoma subtypes diagnosed according to the 2016 WHO renal tumor classification: a study involving 928 patients. Pathol Oncol Res (2017) 23(3):689–98. 10.1007/s12253-016-0179-x
6.
Ficarra V Novara G Galfano A Brunelli M Cavalleri S Martignoni G et al The “Stage, Size, Grade and Necrosis” score is more accurate than the University of California Los Angeles Integrated Staging System for predicting cancer-specific survival in patients with clear cell renal cell carcinoma. BJU Int (2009) 103(2):165–70. 10.1111/j.1464-410X.2008.07901.x
7.
Correa AF Jegede OA Haas NB Flaherty KT Pins MR Adeniran A et al Predicting disease recurrence, early progression, and overall survival following surgical resection for high-risk localized and locally advanced renal cell carcinoma. Eur Urol (2021) 80(1):20–31. 10.1016/j.eururo.2021.02.025
8.
Khene ZE Kutikov A Campi R EAU-YAU Renal Cancer Working Group. Machine learning in renal cell carcinoma research: the promise and pitfalls of “renal-izing” the potential of artificial intelligence. BJU Int (2023) 132(2):231–2. 10.1111/bju.16016
9.
Khene Z Gasmi A Larcher A Bernhard J Doumerc N Ouzaid I et al Validation externe du modèle pronostique assure pour la prédiction des résultats oncologiques des carcinomes rénaux (Rescue Study–UROCCR 88). Progrès en Urologie (2021) 31(13):821. 10.1016/j.purol.2021.08.124
10.
Schmeusser BN Patil DH Nicaise EH Armas-Phan M Nabavizadeh R Narayan VM et al 2018 Leibovich prognostic model for renal cell carcinoma: performance in a large population with special consideration of Black race. Cancer (2024) 130(3):453–66. 10.1002/cncr.35037
11.
Wallace DC . Mitochondria and cancer. Nat Rev Cancer (2012) 12(10):685–98. 10.1038/nrc3365
12.
Gururaja RS . Mitochondrial changes in cancer. In: SinghHSheuSS, editors. Pharmacology of mitochondria. Handbook of experimental pharmacology, 240. Springer International Publishing (2016). p. 211–27. 10.1007/164_2016_40
13.
Warburg O Wind F Negelein E . The metabolism of tumors in the body. J Gen Physiol (1927) 8(6):519–30. 10.1085/jgp.8.6.519
14.
Liberti MV Locasale JW . The Warburg effect: how does it benefit cancer cells?Trends Biochem Sci (2016) 41(3):211–8. 10.1016/j.tibs.2015.12.001
15.
Bose S Zhang C Le A . Glucose metabolism in cancer: the Warburg effect and beyond. Adv Exp Med Biol (2021) 1311:3–15. 10.1007/978-3-030-65768-0_1
16.
Hervouet E Demont J Pecina P Vojtísková A Houstek J Simonnet H et al A new role for the von Hippel-Lindau tumor suppressor protein: stimulation of mitochondrial oxidative phosphorylation complex biogenesis. Carcinogenesis (2005) 26(3):531–9. 10.1093/carcin/bgi001
17.
Semenza GL . HIF-1 mediates the Warburg effect in clear cell renal carcinoma. J Bioenerg Biomembr (2007) 39(3):231–4. 10.1007/s10863-007-9081-2
18.
Gerlinger M Horswell S Larkin J Rowan AJ Salm MP Varela I et al Genomic architecture and evolution of clear cell renal cell carcinomas defined by multiregion sequencing. Nat Genet (2014) 46(3):225–33. 10.1038/ng.2891
19.
Gerlinger M Rowan AJ Horswell S Math M Larkin J Endesfelder D et al Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med (2012) 366(10):883–92. 10.1056/NEJMoa1113205
20.
Brannon AR Reddy A Seiler M Arreola A Moore DT Pruthi RS et al Molecular stratification of clear cell renal cell carcinoma by consensus clustering reveals distinct subtypes and survival patterns. Genes Cancer (2010) 1(2):152–63. 10.1177/1947601909359929
21.
Wallace DC Fan W Procaccio V . Mitochondrial energetics and therapeutics. Annu Rev Pathol (2010) 5:297–348. 10.1146/annurev.pathol.4.110807.092314
22.
Reznik E Miller ML Şenbabaoğlu Y Riaz N Sarungbam J Tickoo SK et al Mitochondrial DNA copy number variation across human cancers. Elife (2016) 5:e10769. 10.7554/eLife.10769
23.
Dardaud LM Bris C Desquiret-Dumas V Boisselier B Tabouret E Mokhtari K et al High mitochondrial DNA copy number is associated with longer survival in young patients with glioblastoma. Neuro-Oncology (2019) 21(8):1084–5. 10.1093/neuonc/noz072
24.
Sourty B Dardaud LM Bris C Desquiret-Dumas V Boisselier B Basset L et al Mitochondrial DNA copy number as a prognostic marker is age-dependent in adult glioblastoma. Neurooncol Adv (2022) 4(1):vdab191. 10.1093/noajnl/vdab191
25.
Lebok P Schütt K Kluth M Witzel I Wölber L Paluchowski P et al High mitochondrial content is associated with breast cancer aggressiveness. Mol Clin Oncol (2021) 15(4):203. 10.3892/mco.2021.2365
26.
Lin CS Lee HT Lee MH Pan SC Ke CY Chiu AWH et al Role of mitochondrial DNA copy number alteration in human renal cell carcinoma. Int J Mol Sci (2016) 17(6):814. 10.3390/ijms17060814
27.
Boucret L Bris C Seegers V Goudenège D Desquiret-Dumas V Domin-Bernhard M et al Deep sequencing shows that oocytes are not prone to accumulate mtDNA heteroplasmic mutations during ovarian ageing. Hum Reprod (2017) 32(10):2101–9. 10.1093/humrep/dex268
28.
Goudenège D Bris C Hoffmann V Desquiret-Dumas V Jardel C Rucheton B et al eKLIPse: a sensitive tool for the detection and quantification of mitochondrial DNA deletions from next-generation sequencing data. Genet Med (2019) 21(6):1407–16. 10.1038/s41436-018-0350-8
29.
Srigley JR Delahunt B Eble JN Egevad L Epstein JI Grignon D et al The international society of urological pathology (ISUP) vancouver classification of renal neoplasia. Am J Surg Pathol (2013) 37(10):1469–89. 10.1097/PAS.0b013e318299f2d1
30.
Fleury C Mignotte B Vayssière JL . Mitochondrial reactive oxygen species in cell death signaling. Biochimie (2002) 84(2-3):131–41. 10.1016/s0300-9084(02)01369-x
31.
Hervouet E Simonnet H Godinot C . Mitochondria and reactive oxygen species in renal cancer. Biochimie (2007) 89(9):1080–8. 10.1016/j.biochi.2007.03.010
32.
Kalyanaraman B Cheng G Hardy M Ouari O Lopez M Joseph J et al A review of the basics of mitochondrial bioenergetics, metabolism, and related signaling pathways in cancer cells: therapeutic targeting of tumor mitochondria with lipophilic cationic compounds. Redox Biol (2018) 14:316–27. 10.1016/j.redox.2017.09.020
33.
Hsu CC Tseng LM Lee HC . Role of mitochondrial dysfunction in cancer progression. Exp Biol Med (Maywood) (2016) 241(12):1281–95. 10.1177/1535370216641787
34.
Guerra F Guaragnella N Arbini AA Bucci C Giannattasio S Moro L . Mitochondrial dysfunction: a novel potential driver of epithelial-to-mesenchymal transition in cancer. Front Oncol (2017) 7:295. 10.3389/fonc.2017.00295
35.
Ricketts CJ De Cubas AA Fan H Smith CC Lang M Reznik E et al The cancer genome atlas comprehensive molecular characterization of renal cell carcinoma. Cell Rep (2018) 23(1):313–26.e5. 10.1016/j.celrep.2018.03.075
36.
Sato Y Yoshizato T Shiraishi Y Maekawa S Okuno Y Kamura T et al Integrated molecular analysis of clear-cell renal cell carcinoma. Nat Genet (2013) 45(8):860–7. 10.1038/ng.2699
37.
Wettersten HI Aboud OA Lara PN Weiss RH . Metabolic reprogramming in clear cell renal cell carcinoma. Nat Rev Nephrol (2017) 13(7):410–9. 10.1038/nrneph.2017.59
38.
Hakimi AA Reznik E Lee CH Creighton CJ Brannon AR Luna A et al An integrated metabolic atlas of clear cell renal cell carcinoma. Cancer Cell (2016) 29(1):104–16. 10.1016/j.ccell.2015.12.004
39.
Du W Zhang L Brett-Morris A Aguila B Kerner J Hoppel CL et al HIF drives lipid deposition and cancer in ccRCC via repression of fatty acid metabolism. Nat Commun (2017) 8(1):1769. 10.1038/s41467-017-01965-8
40.
Nilsson H Lindgren D Mandahl Forsberg A Mulder H Axelson H Johansson ME . Primary clear cell renal carcinoma cells display minimal mitochondrial respiratory capacity resulting in pronounced sensitivity to glycolytic inhibition by 3-Bromopyruvate. Cell Death Dis (2015) 6:e1585. 10.1038/cddis.2014.545
41.
Yu M Shi Y Wei X Yang Y Zhou Y Hao X et al Depletion of mitochondrial DNA by ethidium bromide treatment inhibits the proliferation and tumorigenesis of T47D human breast cancer cells. Toxicol Lett (2007) 170(1):83–93. 10.1016/j.toxlet.2007.02.013
42.
Cavalli LR Varella-Garcia M Liang BC . Diminished tumorigenic phenotype after depletion of mitochondrial DNA. Cell Growth Differ (1997) 8(11):1189–98.
43.
Sun X St John JC . Modulation of mitochondrial DNA copy number in a model of glioblastoma induces changes to DNA methylation and gene expression of the nuclear genome in tumours. Epigenetics and Chromatin (2018) 11(1):53. 10.1186/s13072-018-0223-z
44.
Choueiri TK Tomczak P Park SH Venugopal B Ferguson T Chang YH et al Adjuvant pembrolizumab after nephrectomy in renal-cell carcinoma. N Engl J Med (2021) 385(8):683–94. 10.1056/NEJMoa2106391
45.
Choueiri TK Tomczak P Park SH Venugopal B Ferguson T Symeonides SN et al Overall survival with adjuvant pembrolizumab in renal-cell carcinoma. N Engl J Med (2024) 390(15):1359–71. 10.1056/NEJMoa2312695
46.
Kim H Komiyama T Inomoto C Kamiguchi H Kajiwara H Kobayashi H et al Mutations in the mitochondrial ND1 gene are associated with postoperative prognosis of localized renal cell carcinoma. Int J Mol Sci (2016) 17(12):2049. 10.3390/ijms17122049
47.
Kwon TJ Ro JY Mackay B . Clear-cell carcinoma: an ultrastructural study of 57 tumors from various sites. Ultrastruct Pathol (1996) 20(6):519–27. 10.3109/01913129609016356
48.
Mackay B Ordónez NG Khoursand J Bennington JL . The ultrastructure and immunocytochemistry of renal cell carcinoma. Ultrastruct Pathol (1987) 11(5-6):483–502. 10.3109/01913128709048445
49.
Erlandson RA Shek TW Reuter VE . Diagnostic significance of mitochondria in four types of renal epithelial neoplasms: an ultrastructural study of 60 tumors. Ultrastruct Pathol (1997) 21(5):409–17. 10.3109/01913129709021939
50.
Tickoo SK Amin MB Linden MD Lee MW Zarbo RJ . Antimitochondrial antibody (113-1) in the differential diagnosis of granular renal cell tumors. The Am J Surg Pathol (1997) 21(8):922–30. 10.1097/00000478-199708000-00006
51.
Nilsson H Lindgren D Axelson H Brueffer C Saal LH Lundgren J et al Features of increased malignancy in eosinophilic clear cell renal cell carcinoma. J Pathol (2020) 252(4):384–97. 10.1002/path.5532
52.
Yoshida T Ohe C Ikeda J Atsumi N Ohsugi H Sugi M et al Eosinophilic features in clear cell renal cell carcinoma correlate with outcomes of immune checkpoint and angiogenesis blockade. J Immunother Cancer (2021) 9(9):e002922. 10.1136/jitc-2021-002922
53.
Yang XJ Takahashi M Schafernak KT Tretiakova MS Sugimura J Vogelzang NJ et al Does “granular cell” renal cell carcinoma exist? Molecular and histological reclassification. Histopathology. (2007) 50(5):678–80. 10.1111/j.1365-2559.2007.02626.x
54.
Dagher J Kammerer-Jacquet SF Brunot A Pladys A Patard JJ Bensalah K et al Wild-type VHL clear cell renal cell carcinomas are a distinct clinical and histologic entity: a 10-year follow-up. Eur Urol Focus (2016) 1(3):284–90. 10.1016/j.euf.2015.06.001
55.
Batavia AA Schraml P Moch H . Clear cell renal cell carcinoma with wild-type von Hippel-Lindau gene: a non-existent or new tumour entity?Histopathology (2019) 74(1):60–7. 10.1111/his.13749
56.
Moch H Amin MB Berney DM Compérat EM Gill AJ Hartmann A et al The 2022 world health organization classification of tumours of the urinary system and male genital organs-Part A: renal, penile, and testicular tumours. Eur Urol (2022) 82(22):458–68. 10.1016/j.eururo.2022.06.016
57.
Trpkov K Hes O Williamson SR Adeniran AJ Agaimy A Alaghehbandan R et al New developments in existing WHO entities and evolving molecular concepts: the Genitourinary Pathology Society (GUPS) update on renal neoplasia. Mod Pathol (2021) 34(7):1392–424. 10.1038/s41379-021-00779-w
58.
Trpkov K Williamson SR Gill AJ Adeniran AJ Agaimy A Alaghehbandan R et al Novel, emerging and provisional renal entities: the Genitourinary Pathology Society (GUPS) update on renal neoplasia. Mod Pathol (2021) 34(6):1167–84. 10.1038/s41379-021-00737-6
59.
Somorácz Á Kuthi L Micsik T Jenei A Hajdu A Vrabély B et al Renal cell carcinoma with clear cell papillary features: perspectives of a differential diagnosis. Pathol Oncol Res (2020) 26(3):1767–76. 10.1007/s12253-019-00757-3
60.
Gilkerson R Bravo L Garcia I Gaytan N Herrera A Maldonado A et al The mitochondrial nucleoid: integrating mitochondrial DNA into cellular homeostasis. Cold Spring Harb Perspect Biol (2013) 5(5):a011080. 10.1101/cshperspect.a011080
61.
Farge G Falkenberg M . Organization of DNA in mammalian mitochondria. Int J Mol Sci (2019) 20(11):E2770. 10.3390/ijms20112770
62.
Farge G Mehmedovic M Baclayon M van den Wildenberg SMJL Roos WH Gustafsson CM et al In vitro-reconstituted nucleoids can block mitochondrial DNA replication and transcription. Cell Rep (2014) 8(1):66–74. 10.1016/j.celrep.2014.05.046
63.
Pérez-Escuredo J Dadhich RK Dhup S Cacace A Van Hée VF De Saedeleer CJ et al Lactate promotes glutamine uptake and metabolism in oxidative cancer cells. Cell Cycle (2016) 15(1):72–83. 10.1080/15384101.2015.1120930
64.
Corbet C Draoui N Polet F Pinto A Drozak X Riant O et al The SIRT1/HIF2α axis drives reductive glutamine metabolism under chronic acidosis and alters tumor response to therapy. Cancer Res (2014) 74(19):5507–19. 10.1158/0008-5472.CAN-14-0705
65.
Yoo HC Yu YC Sung Y Han JM . Glutamine reliance in cell metabolism. Exp Mol Med (2020) 52(9):1496–516. 10.1038/s12276-020-00504-8
66.
Linehan WM Schmidt LS Crooks DR Wei D Srinivasan R Lang M et al The metabolic basis of kidney cancer. Cancer Discov (2019) 9(8):1006–21. 10.1158/2159-8290.CD-18-1354
67.
Debnath J . Detachment-induced autophagy during anoikis and lumen formation in epithelial acini. Autophagy (2008) 4(3):351–3. 10.4161/auto.5523
68.
Yoo HC Park SJ Nam M Kang J Kim K Yeo JH et al A variant of SLC1A5 is a mitochondrial glutamine transporter for metabolic reprogramming in cancer cells. Cell Metab. (2020) 31(2):267–83. 10.1016/j.cmet.2019.11.020
69.
Emberley E Pan A Chen J Dang R Gross M Huang T et al The glutaminase inhibitor telaglenastat enhances the antitumor activity of signal transduction inhibitors everolimus and cabozantinib in models of renal cell carcinoma. PLoS One (2021) 16(11):e0259241. 10.1371/journal.pone.0259241
70.
Raczka AM Reynolds PA . Glutaminase inhibition in renal cell carcinoma therapy. Cancer Drug Resist (2019) 2(2):356–64. 10.20517/cdr.2018.004
Summary
Keywords
clear cell renal cell carcinoma, mtDNA copy number, prognosis, 786-O cell line, ethidium bromide, eosinophilic clear cell renal cell carcinoma, mitochondrial genome
Citation
Bellal S, Rolley C, Richard J, Bounaix N, Le Corre V, Copin M-C, Blanchet O, Bigot P, Procaccio V and Bris C (2025) MtDNA copy number enrichment is associated with poor prognosis and eosinophilic morphology in clear cell renal cell carcinoma. Pathol. Oncol. Res. 31:1612172. doi: 10.3389/pore.2025.1612172
Received
10 May 2025
Accepted
25 June 2025
Published
23 July 2025
Volume
31 - 2025
Edited by
Andrea Ladányi, National Institute of Oncology (NIO), Hungary
Updates
Copyright
© 2025 Bellal, Rolley, Richard, Bounaix, Le Corre, Copin, Blanchet, Bigot, Procaccio and Bris.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah Bellal, sarah.bellal@chu-angers.fr
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.