Abstract
Many subtypes of bone and soft tissue tumours harbour specific chromosome translocations leading to chimeric fusion genes. The identification of these specific fusion genes is the basis of molecular diagnoses in such tumours. Break-apart FISH is a robust method that is commonly used to identify these translocations and provide diagnostic support to histological interpretations. The signal patterns of the break-apart probes are usually easily interpreted. However, some cases show abnormal signal patterns leading to equivocal and challenging interpretation. The incidence of these abnormal patterns is largely unknown. Using a retrospective cohort we explored the incidence of abnormal signal patterns across common bone and soft tissue tumour types to raise awareness of this occurrence and to aid in the interpretation. In total, 1,087 bone and soft tissue tumours tested by break-apart probes were examined. The abnormal signal patterns were classified as deletion, additional copy and amplification, which were found at highest frequency in low-grade fibromyxoid sarcoma (32%, 6/19), and at moderate frequencies in those from alveolar rhabdomyosarcoma (10%, 9/94), nodular fasciitis (9%, 18/209), synovial sarcoma (8%, 17/207) and Ewing sarcoma/round cell sarcoma with EWSR1-non-ETS fusions (6%, 29/497). The lowest frequency was found in clear cell sarcoma (1%, 1/61). Despite the equivocal results from the abnormal signal patterns, the specific fusion genes were confirmed by orthogonal molecular techniques such as FISH with fusion probes, RT-PCR or next-generation sequencing.
Introduction
The accurate diagnosis and subsequent clinical management of many bone and soft tissue tumours are reliant on molecular testing. Many of these tumours have characteristic genetic translocations (Table 1) [1–4], which can be detected by fluorescence in situ hybridization (FISH), reverse transcription polymerase chain reaction (RT-PCR) and Next-Generation Sequencing (NGS).
TABLE 1
| Type of tumour | Chromosome abnormality | Gene involved | Frequency | Break-apart probe |
|---|---|---|---|---|
| Alveolar rhabdomyosarcoma Clear cell sarcoma Ewing sarcoma/PNET Round cell sarcoma with EWSR1-non-ETS fusions Low grade fibromyxoid sarcoma Nodular fasciitis Synovial sarcoma |
t (2; 13) (q35; q14) t (1; 13) (p36:q14) t (12; 22) (q13; q12) t (2; 22) (q34; q12) t (10; 22) (p11; q12) t (11; 22) (q24; q12) t (21; 22) (q22; q12) t (20; 22) (q13; q12) t (7; 16 (q34; p11) t (11; 16) (p11; p11) t (17; 22) (p13; q13) t (x; 18) (p11; q11) |
PAX3::FOXO1
PAX7::FOXO1 EWSR1::ATF1 EWSR1::CREB1 EWSR1::CREM EWSR1::FLI1 EWSR1::ERG EWSR1::NFATC2 FUS::CREB3L2 FUS::CREB3L1 MYH9::USP6 SS18::SSX1 SS18::SSX2 SS18::SSX4 |
85% 10% 90% 10% rare 85% 10% <1% 90% 5% 90% 90% 10% rare |
FOXO1 EWSR1 EWSR1 FUS USP6 SS18 |
Chromosome translocation in bone and soft tissue tumours.
The signal patterns of the break-apart probes are usually easily interpreted. However, some cases may show abnormal signal patterns leading to challenging interpretation, equivocal results and therefore uncertainty in diagnosis and management. Several studies have systemic examined abnormal signal patterns in bone and soft tissue tumours [5–7], however, the true incidence and significance of the abnormal signal patterns in different subtypes are unknown.
The present study aims to explore the incidence of abnormal signal patterns by tumour type to raise awareness of this occurrence and correlate with genomic sequencing where available.
Materials and methods
A total of 1,087 samples were retrieved from our files in the Department of Cellular and Molecular Pathology, Royal National Orthopaedic Hospital (Table 2). They included 94 cases of alveolar rhabdomyosarcoma (ARMS), 61 cases of clear cell sarcoma (CCS), 497 cases of Ewing sarcoma/round cell sarcoma with EWSR1-non-ETS fusions, 19 cases of low-grade fibromyxoid sarcoma (LGFMS), 209 cases of nodular fasciitis (NF) and 207 cases of synovial sarcoma (SS). All cases were classified according to the World Health Organization classification (WHO) of bone and soft tissue tumours [1]. All cases analysed by FISH using break-apart probes were reviewed to identify the frequency and type of abnormal signal patterns. These were classified as deletion, amplification, and extra copy of the gene locus.
TABLE 2
| Type | ARMS (FOXO1) | CCS (EWSR1) | ES/RCSEEF | LGFMS (FUS) | NF (USP6) | SS (SS18) |
|---|---|---|---|---|---|---|
| No. of cases | 94 | 61 | 497 | 19 | 209 | 207 |
| Deletion | 0 | 0 | 8 (2%) | 0 | 16 (8%) | 8 (4%) |
| Extra copy | 0 | 1 (2%) | 15 (3%) | 6 (32%) | 2 (1%) | 9 (4%) |
| Amplification | 9 (10%) | 0 | 6 (1%) | 0 | 0 | 0 |
| Fusion gene detected by FISHa/RT-PCRa/NGSb/WGSb | 3/9 PAX3::FOXO1 (+)a 6/9 PAX7::FOXO1 (+)a |
1/61 EWSR1::CREM (+)b | 12/29 EWSR1::FLI1 (+)a,b 9/29 EWSR1::ERG (+)a,b 6/29 EWSR1:NFATC2 (+)a,b 1/29 EWSR1::FLI1(ERG) (−)a 1 case no material available |
4/6 FUS::CREB3L2 (+)a 2/6 FUS::CREB3L2 (−)a |
11/18 MYH9::USP6 (+)a,b 1/18 FRMD6::USP6 (+)b 5/18 MYH9::USP6 (−)a 1 case no material available |
13/17 SS18::SSX1 (+)a,b 3/17 SS18::SSX2 (+)a,b 1 case no material available |
Abnormal signal pattern of break-apart probe and fusion gene detected.
Note: ARMS, alveolar rhabdomyosarcoma; CCS, clear cell sarcoma; ES, ewing sarcoma; RCSEEF, round cell sarcoma with EWSR1-non-ETS fusion; LGFMS, low grade fibromyxoid sarcoma; NF, nodular fasciitis; SS, synovial sarcoma.
FISH/RT-PCR assay.
NGS, Next-Generation Sequencing/WGS, whole genome sequencing.
Fluorescence in situ hybridization (FISH)
FISH analysis was performed on formalin fixed paraffin embedded sections using dual color break-apart probes, namely EWSR1, FOXO1, FUS, SS18 (Abbott Molecular, USA), NFATC2 (Agilent Technologies, California, USA) and USP6 (ZytoVision, Bremerhaven, Germany). Fusion FISH probes of PAX3::FOXO1, PAX7::FOXO1, EWSR1::FLI1 (ZytoVision, Germany) and EWSR1::NFATC2 (Wuhan Kanglu Biotechnology Co., Ltd, China) were used as an alternative method to confirm the translocation in a spectrum of equivocal cases. The procedure of FISH assay was described previously [8]. After dewaxing in xylene and rehydration in a series of ethanol, sample sections were cooked in a pressure cooker for 5 min in deionized water. Then the sections were digested in 0.125% pepsin solution at 37°C for 50 min. The specific break-apart probe was co-denatured on the sections at 72°C for 15 min and hybridized at 45°C overnight in a humidified box in an oven. Post hybridization washings were carried out and counterstained with 4.’6′- diamidino-2-phenylindole from Vector Laboratories (Burlingame, CA, United States). Fifty non-overlapping nuclei were counted for each case. The typical positive signal pattern was interpreted as 1 yellow, 1 red and 1 green and if the green and a red signal were separated by more than two times distance of the size of one signal in more than 15% of the counted cells. The abnormal signal patterns were classified as a deletion, amplification, and extra copy of the gene locus. When 1 yellow and 1 to a few green signals without a red signal/or 1 yellow and 1 to a few red signals without green signal were considered as a deletion. If the number of green/or red signals were too numerous to be counted it was considered as an amplification. If 2 or more yellows and 1 to few greens without red signal or 2 or more yellows and 1 to few reds without a green signal were considered as an extra copy of the gene. An abnormal signal pattern is considered if more than 15% counted cells showing same abnormal signal pattern.
RNA extraction and reverse transcription
RNA was extracted from 10 µm sections cut from paraffin-embedded resection or biopsy samples. FFPE Ambion Recoverall Total Nucleic Acid isolation kit (Invitrogen, Thermo Fisher Scientific, United States). Between 1 and 3 µL of the RNA samples were reverse transcribed using Superscript III First-Strand Synthesis kit (Invitrogen, Thermo Fisher Scientific, United States) using random hexamers. All steps were performed according to the manufacturer instructions.
Conventional polymerase chain reaction
PCR amplification was performed on duplicate samples of 1 µL aliquots of cDNA using specific primer sets designed based on the known fusion genes and break points (all primers and product sizes shown in Table 3). Reactions were performed in 25 µL using 1 × buffer II, 200 µM of each dNTP, 5 pmol of each primer, 1.5 mM MgCI2, and 1 U of Platinum Taq DNA polymerase (Applied biosystems, Thermo Fisher Scientific, United States). A touchdown protocol was used with cycling parameters as follows: 7 min at 95°C followed by 45 s at 94°C, 45 s at 66°C, 1 min 30 s at 72°C which was followed by reducing the annealing temperature by 1°C each cycle to 57°C (10 cycles), followed by 30 cycles at 56°C and finally 5 min at 72°C [5].
TABLE 3
| Strand primer sequence 5’ – 3′ | Product size (bp) |
|---|---|
| G6PD primers G6PD 86 Sense ACGGCAACAGATACAAGAAC G6PD 141 Sense CCAAGAAGCCGGGCATGT G6PD 200 Sense GCGCAACGAGCTGGTGAT G6PD Anti-sense CGAAGTGCATCTGGCTCC EWSR1 exon7 Sense CTGGATCCTACAGCCAAGCTCCAAG FLI1 exon6 Anti-sense GTTGAGGCCAGAATTCATGTTA ERG exon7 Anti-sense ACCGGTCCAGGCTGATCT ERG exon10 Anti-sense AACTGCCAAAGCTGGATCTG FUS exon6 Sense GCTATGAACCCAGAGGTCGT CREB3L2 exon5 Anti-sense TTATGAGGAGCCGTGAGGAG MYH9 exon1 Sense GGGGCAGATCCAGGTTCAG USP6 exon1 Anti-sense GAAACTGGGCATCTCTGTGGC USP6 exon2 Anti-sense GATGGACATGGTAGAGAATGC PAX3 Sense CCGACAGCAGCTCTGCCTAC PAX7 Sense CCGACAGCAGCTCTGCCTAC FOXO1 Anti-sense TGAACTTGCTGTGTAGGGACAG SS18 Sense AGACCAACACAGCCTGGACCAC SSX1 Anti-sense ACACTCCCTTCGAATCATTTTCG SSX2 Anti-sense GCACTTCCTCCGAATCATTTC |
86 141 200 Type I: 125, type II: 191 94 81 64 to 121 208 173 169 160 108 108 |
Primers and expected product sizes of RT-PCR.
PCR products were analyzed by electrophoresis on 8% polyacrylamide gels, stained with GelRed and visualized under UV illumination using a Syngene NuGenius Gel imaging system (Cambridge, UK). Samples yielding PCR products of the predicted size in both reactions were considered as positive. A negative (no template) and positive controls of the specific fusion genes confirmed by sequencing were used for each experiment.
The housekeeping gene of glucose-6-phosphase dehydrogenase (G6PD) was amplified in parallel using the same reaction conditions. The PCR primers were designed to provide the template for generation of products of 86, 141 and 200 bp, which are the controls for RNA quality of the samples.
Next-generation sequencing (NGS)
FFPE samples were referred to a centralized Genomic Laboratory Hub to perform targeted RNA sequencing (RNAseq).
Whole-genome sequencing
High quality DNA was extracted from frozen tissue using QIAamp DNA mini kit (Qiagen, Hilden, Germany). Both tumour and matching normal samples were sequenced using the Novoseq (Illumina Inc.) using a PCR free workflow.
The tumour samples were sequenced to a depth of 70X and normal/germline to 30X. Fastq files were QC’ed, aligned and pre-processed using bcbio-nextgen pipeline [9]. The three SV callers – Manta [10], GRIDSS2 [11], and Svaba [12] were used to determine the structural variants (SVs), and the final agreement was reached by considering calls from at least two out of three callers.
Results
Break-apart FISH analysis was performed in 1,087 cases demonstrating informative results in Table 2; Figures 1–6, including 94 ARMS, 61 CCS, 497 Ewing sarcoma/round cell sarcoma with EWSR1-non-ETS fusions, 19 LGFMS, 209 NF and 207 SS. The summary of abnormal signal patterns is shown in Table 2. Abnormal signal patterns were detected in 7% (80/1,087 cases), including 10% (9/94 cases) of ARMS (FOXO1) (Figure 2), 1% (1/61 cases) of CCS (EWSR1) (Figure 6), 6% (29/497 cases) of Ewing sarcoma/round cell sarcoma with EWSR1-non-ETS fusions (EWSR1) (Figures 3, 5, respectively), 32% (6/19 cases) of LGFMS (FUS), 9% (18/209 cases) of NF (USP6) and 8% (17/207 cases) of SS (SS18) (Figure 4).
FIGURE 1
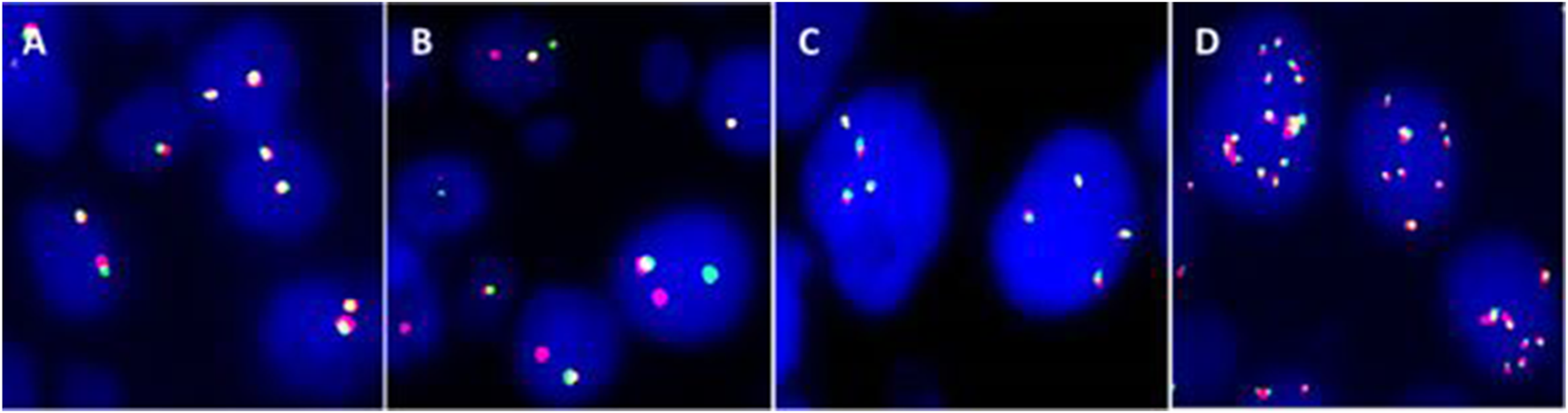
Usual signal pattern of break-apart probe. (A) Negative signal pattern of two yellow signals. (B) Positive signal pattern of one yellow and a break-apart (one green separated from one red). (C) Negative: Three to 4 copies of yellow signals. (D) Negative: Multi-copies of yellow signals.
FIGURE 2
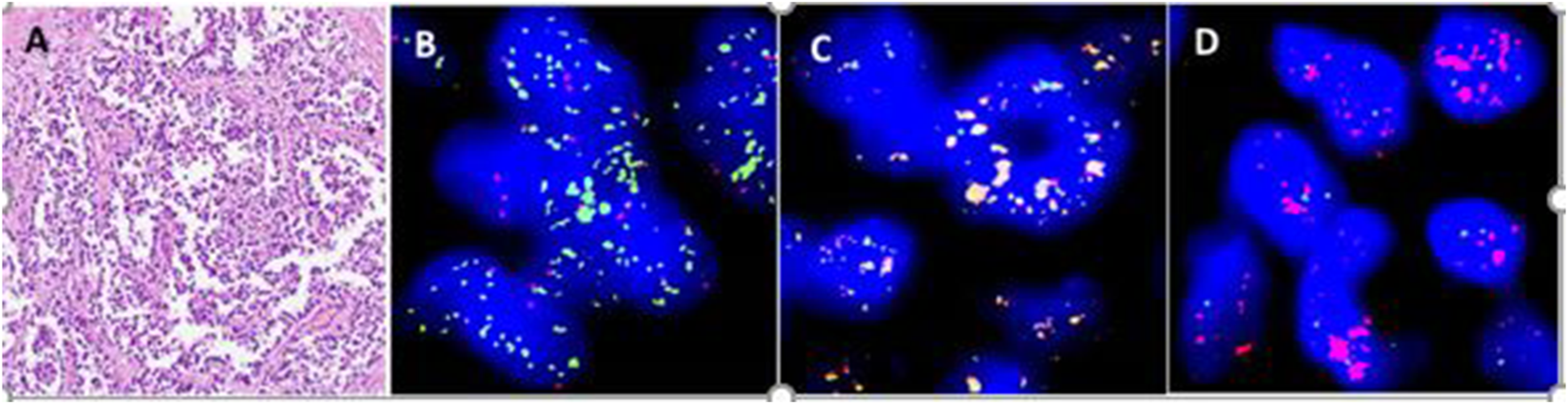
An alveolar rhabdomyosarcoma with FOXO1 gene amplification. (A) Round cells with pseudoalveolar pattern. (B)FOXO1 break-apart probe shows positive signal pattern with amplification of 3′ end of the FOXO1 locus (Green). (C) Multi fusion yellow signals of PAX7::FOXO1 by FISH of PAX7::FOXO1 fusion probe. (D) No fusion signal found by FISH of PAX3::FOXO1 fusion probe.
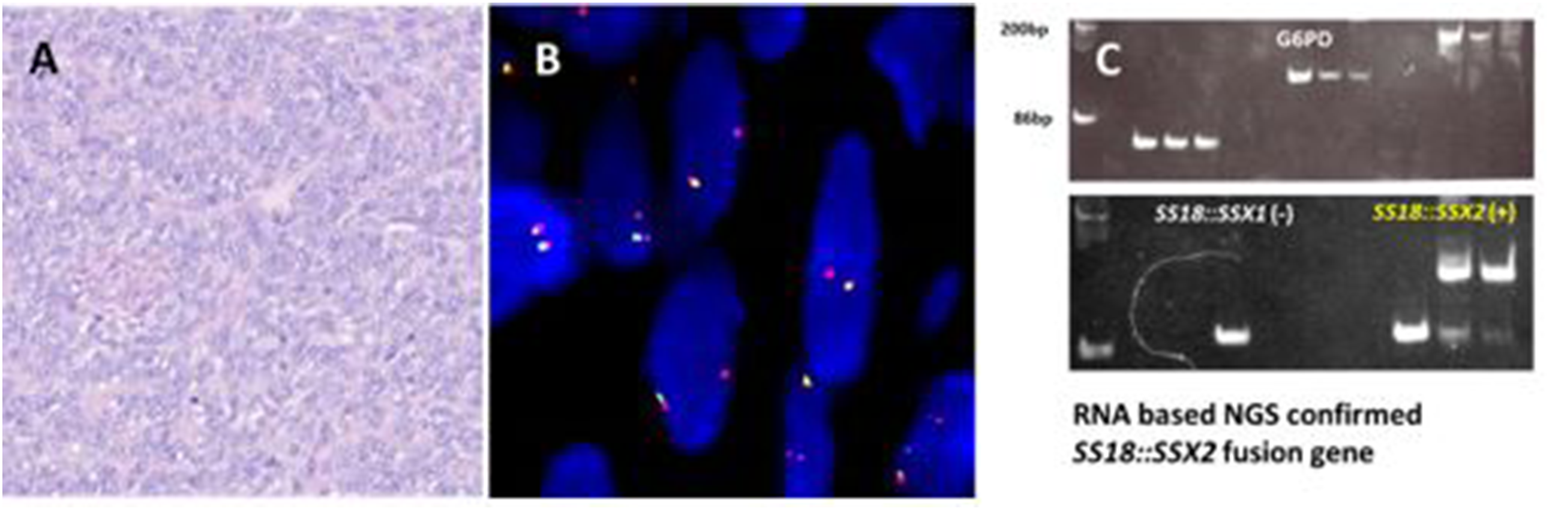
FIGURE 3
A NFATC2-rearranged sarcoma with EWSR1 gene amplification. (A) Undifferentiated blue small round cells composed of cords of cells in a fibrous stroma. (B)EWSR1 break-apart probe shows atypical signal pattern: amplification of 5′ end of the EWSR1 locus. (C) NFATC2 break-apart probe confirmed NFATC2 gene rearranged with amplification of 3′ end of the NFATC2 locus. EWSR1::NFATC2 fusion gene detected by NGS.
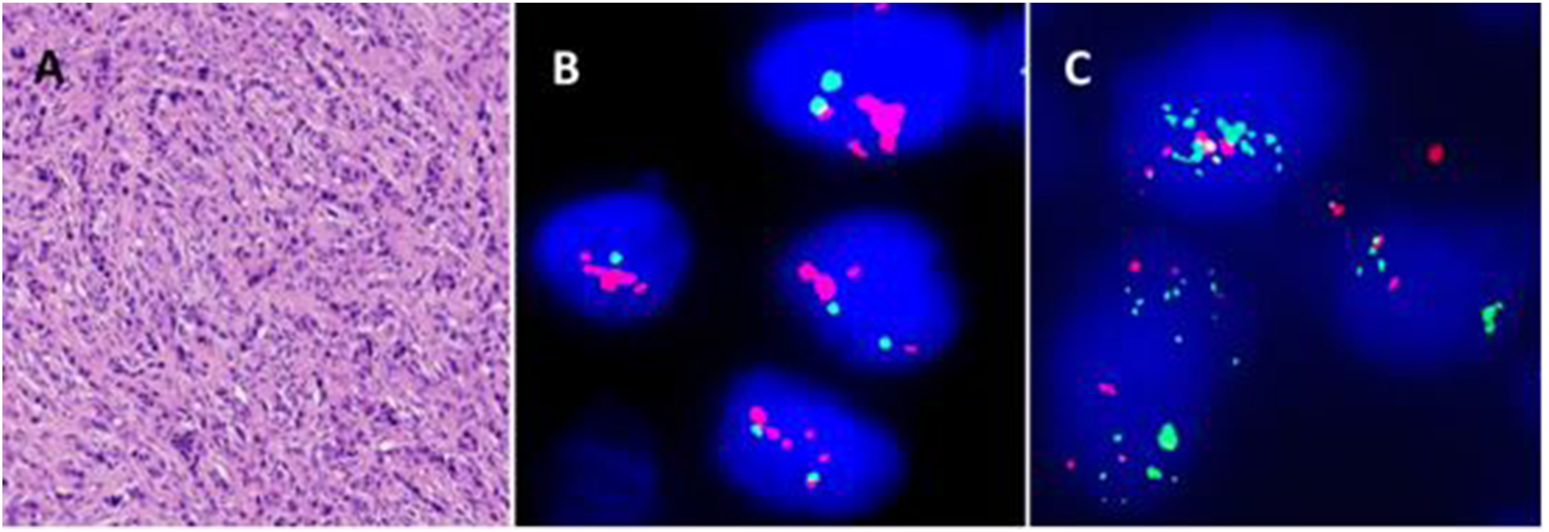
FIGURE 4
A synovial sarcoma with deletion of 3′ end of SS18 locus. (A) Monophasic-type SS. (B)SS18 break-apart probe shows atypical signal pattern of one yellow and one red signals: deletion of 3′ end of the SS18 locus. (C)SS18::SSX2 fusion gene detected by RT-PCR and NGS.
FIGURE 5
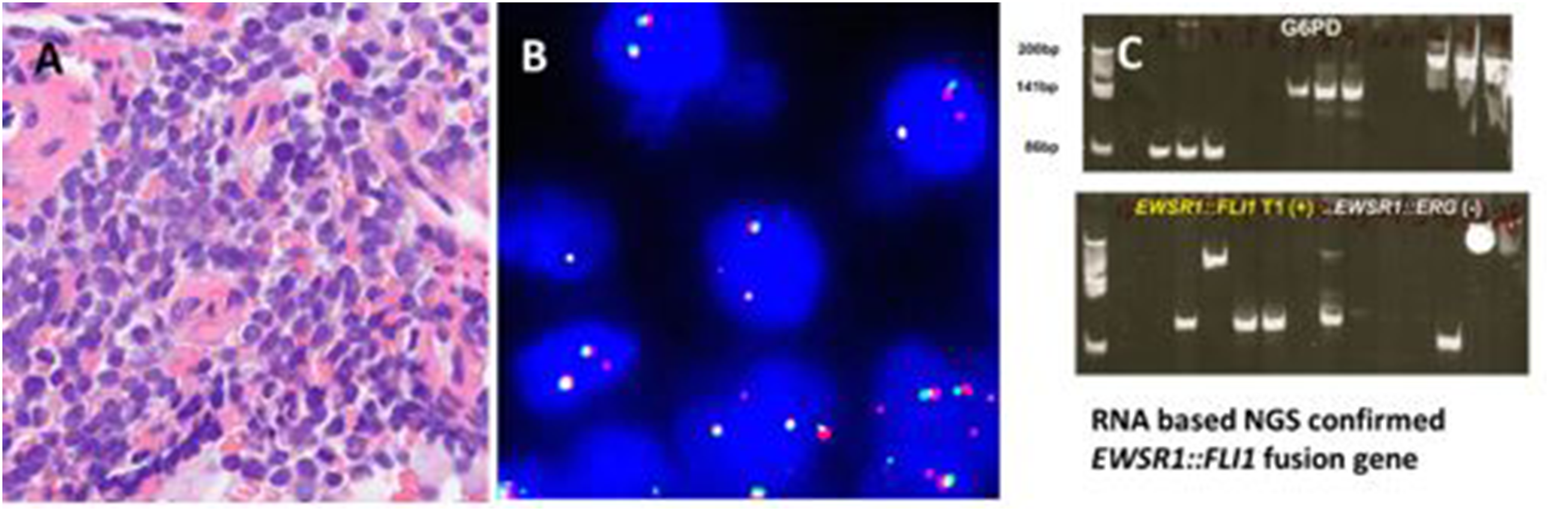
An Ewing sarcoma with no break-apart and an extra copy of EWSR1 gene locus. (A) Monomorphic small blue round cell tumour. (B)EWSR1 break-apart probe shows atypical signal pattern of two yellow and one red signals: one extra copy of the 5′ end of the EWSR1 locus. (C)EWSR1::FLI1 type I fusion gene detected by RT-PCR and NGS.
FIGURE 6
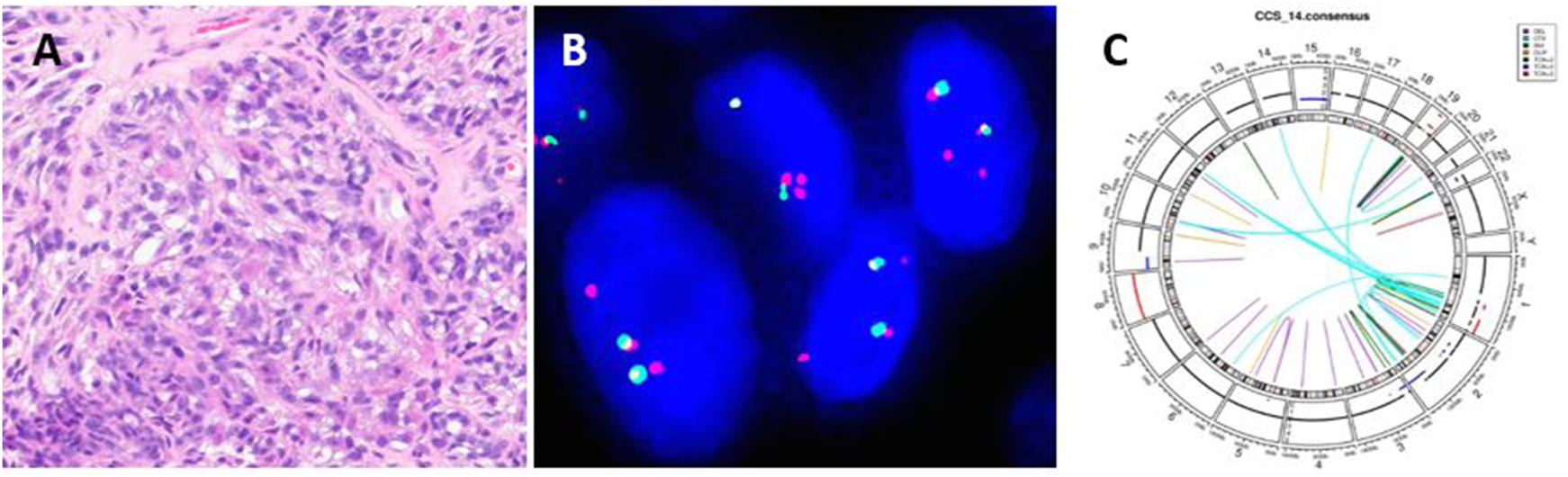
A clear cell sarcoma with extra copies of 5′ end of EWSR1 locus. (A) Polygonal cells with vesicular nuclei and cytoplasmic clearing forming sheets and nests. (B)EWSR1 break-apart probe shows atypical signal pattern of two yellow and two red signals: extra copy of 5′ end of the EWSR1 locus. (C) Circos plot of EWSR1::CREM fusion gene detected by WGS.
The typical pattern of break-apart probe signals in an interphase nucleus without a gene rearrangement are two yellow signals (red/green overlapping signals) which represent two normal gene loci (Figure 1A). A signal pattern consisting of one yellow signal, split signal pattern of one red signal and a separated green signal in a nucleus indicates a typical positive signal pattern (Figure 1B). Multiple yellow signals without separate red and green signals are considered as negative (Figures 1C,D).
94 putative ARMS were screened by FOXO1 break-apart probe for FOXO1 gene rearrangement (Figure 2A). The average age of ARMS patients was 30 years (range 1–85 years) with a 1:1 male to female ratio. The most common site of occurrence was the extremities (25, 27%) and nasal cavity (20, 21%). Most of cases displayed the split pattern of separate red and green signals, however, 9 cases demonstrated FOXO1 amplification with few yellow signals, 1 to 2 red and amplification of 3′ of the FOXO1 locus of more than 15 copies of green signals (Figure 2B). Three of 9 cases carrying the PAX3::FOXO1 fusion gene were confirmed by PAX3::FOXO1 fusion probe. PAX7::FOXO1 fusion gene was detected in six of 9 cases by PAX7::FOXO1 fusion probe (Table 2; Figures 2C,D). Among these 9 cases with an amplification signal pattern, the majority of cases were female (6). Six of 9 cases were from the extremities. No deletion or extra copy of FOXO1 locus was found in any of the 94 cases of alveolar rhabdomyosarcomas screened.
61 CCS were screened for an EWSR1 gene rearrangement (Figure 6A). The average age of CCS patients was 34 years (range 9–73 years) with a 1:1.6 male to female ratio. The most common site of occurrence was the distal lower extremities (39, 64%). Nearly all cases showed the typical positive signal pattern of 1 yellow, 1 red and 1 separated green except one case (2%, 1/61 cases) which displayed an extra copy of EWSR1 locus with 2 yellow and 2 red signals (Figure 6B). This case demonstrated the rare EWSR1::CREM fusion which was identified by both RNAseq NGS and WGS (Figure 6C). No deletion or amplification of EWSR1 locus was found in any of the clear cell sarcoma cases assessed.
A total of 497 Ewing sarcoma/round cell sarcoma with EWSR1-non-ETS fusions were tested for the EWSR1 gene rearrangement (Table 2). The average age of ES/round cell sarcoma with EWSR1-non-ETS fusions patients was 23 years (range 1–87 years) with a 1.7:1 male to female ratio. 57% of the patients were <20 years old at diagnosis. The most common sites of involvement were long bone in 40% (199/497), followed by pelvis 16% (81/497) and ribs 8% (40/497). Abnormal signal patterns were detected in 29 (6%, 29/497) cases. These included 8 cases (2%, 8/497) which showed a deletion pattern with 1 yellow and 1 to 2 red signals of 5′ end of the EWSR1 locus, 15 cases (3%, 15/497) with an extra copy with 2 yellow and 1 to 4 red signals (Figure 5), and 6 cases (1%, 6/497) showing 1 yellow, 1 green and amplification of 5′ end of the EWSR1 locus with more than 8 to 20 copies of red signals (Figure 3). Among 8 cases displaying the deletion signal pattern, the EWSR1::FLI1 fusion was proved in 5 cases by FISH, RT-PCR or NGS, whilst the EWSR1::ERG fusion gene was identified in 2 cases. One case had no remaining material available for further testing. In the 15 cases showing extra copy abnormal signal patterns, the EWSR1::FLI1 fusion gene was detected in 7 cases by FISH, RT-PCR or NGS (Figure 5). The EWSR1::ERG fusion gene was found in 7 cases by RT-PCR or NGS. The EWSR1::NFATC2 fusion gene was detected by FISH and NGS in all 6 cases with the amplification of 5′ end of EWSR1 locus (Figure 3). Six cases (40%, 6/15) with extra copy of EWSR1 locus were from the femur. Four cases (67%, 4/6) showing EWSR1 amplification of 5′ end of the EWSR1 locus were from tumours in the femur. No specific anatomical site was identified in the 8 cases with deletion signal pattern.
19 LGFMS were retrieved for evaluation using the FUS break-apart probe. The average age of LGFMS patients was 44 years (range 4–76 years) with a 1.4:1 male to female ratio. 68% (13/19) of the patients were >40 years old at the time of diagnosis. The most common sites of occurrence were the trunk (42%, 8/19) and proximal extremity (26%, 5/19). Among LGFMS, 32% (6/19) cases demonstrated abnormal signal patterns of extra copies with 2–4 yellow and extra copy of 5′ end of FUS locus with 1–2 green signals (Table 2). The FUS::CREB3L2 fusion gene was detected in 4 cases by RT-PCR and not detected in 2 cases. No deletion or amplification of FUS locus was detected in 19 LGFMS detected.
Regarding the USP6 gene rearrangement in 209 NF, the average age of NF patients was 37 years (range 3–81 years) with a 1.1:1 male to female ratio. The most common sites of occurrence were upper extremities (32%, 67/209), followed by trunk (21%, 44/209), head (11%, 24/209) and neck (10%, 20/209). 18 (9%) of 209 patient samples showed abnormal signal patterns of deletion (16 cases) with patterns of 1 yellow and 1 red signal (15 cases) or 1 yellow and 1 green signal (1 case). 2 cases showed extra copies using the USP6 break-apart probe, with 2 yellow and 1 green signal in a case, and 2 yellow and 1 to 4 red signals in another case. Among these 18 cases with abnormal signal patterns, the MYH9::USP6 fusion gene was identified by RT-PCR and NGS in 11 cases (61%). FRMD6::USP6 fusion gene was found by NGS in 1 case which had extra copy with 2 yellow and 1 to 4 red signals. MYH9::USP6 fusion gene was not detected in 5 cases by RT-PCR. One case had no remaining material available for further testing.
207 SS were analysed using the SS18 break-apart probe, the average age of SS patients was 43 years (range 8–91 years) with a 1.1 male to female ratio. 67% (57/207) of the patients were below the age of 50 years. The most common sites of occurrence were extremities (65%, 134/207), followed by trunk (20%, 42/207), head and neck (4%, 9/207). 17 cases (8%) showed abnormal signal patterns of deletion of 3′ end of the SS18 locus (8 cases) and extra copies of the SS18 locus (9 cases). No amplification of SS18 locus was identified. Among these 17 cases, SS18::SSX1 and SS18::SSX2 fusion genes were found in 13 cases (76%) and 3 cases (18%) by RT-PCR or NGS, respectively.
Discussion
Current techniques such as panel NGS testing and WGS have advanced the classification of bone and soft tissue tumours and enabled a more comprehensive understanding of disease pathogenesis [1]. However, these techniques require specialized equipment, trained bioinformaticians and clinical scientists, and high quality material with high levels of tumour purity. Moreover, the turnaround times are slower than traditional techniques. RT-PCR is a relatively simple, and sensitive molecular assay to detect specific known fusion genes. However, RT-PCR may not be able to detect novel fusion genes due to variability in the transcriptome and variations of translocation partners. Ewing sarcoma with EWSR1 gene rearrangement is presented as a prototypical example [13]. The breakpoints are variable in the introns of the EWSR1 gene. The multiple fusion partners of EWSR1 gene associated with Ewing sarcoma are FLI1, ERG, ETV1, ETV4, FEV and ZSG. Interphase FISH is rapid and can serve as a first line assay to detect the gene rearrangement in the routine pathological diagnostic workup of bone and soft tissue tumours. Fusion probes are used to support clinical diagnoses by detecting specific fusion genes when the abnormal signal patterns are observed by break-apart probes. However, the range of commercially available fusion probes is relatively less common and the signal patterns detected by break-apart probes are much more easily interpreted than those of fusion probes.
The frequency of abnormal signal patterns of break-apart probes in sarcomas are largely undescribed in the literature but poses a dilemma for clinical scientists. Papp, et al summarized 301 cases of soft tissue sarcomas with unusual signal patterns [6]. They found that 14% of sarcomas including ARMS, CCS, Ewing sarcoma, myxoid liposarcoma, LGFMS, NF and SS had unusual signal patterns. They considered deletion (1 yellow and 1 red/green), extra copy (2 yellow and 1-2 red or 1-2 green) and amplification as atypical signal patterns. However, the cases with a break-apart signal plus 1 additional yellow or 1 red signal were also considered as atypical signal patterns which are different from our classification of abnormal signal patterns. We classified the deletion, extra copy and amplification as three different types of abnormal signal patterns. If the cases showed a typical separated green and red signal regardless of additional few yellow or few red or few green signals, we considered these as positive gene rearrangements rather than the abnormal signal patterns.
In our present study, we retrospectively reviewed the FISH results from our routine diagnostic service using break-apart probes from 1,087 patient samples. In total, 80 (7%) of the 1,087 tumours had abnormal signal patterns (Table 2). From the soft tissue sarcomas cohort, we found abnormal patterns in alveolar rhabdomyosarcoma. A recurrent t (2; 13) (q35; q14)PAX3::FOXO1 or t (1; 13) (p36; q14)PAX7::FOXO1 chromosomal translocations are associated with alveolar rhabdomyosarcoma [1]. PAX3::FOXO1 fusion gene is detected in 85% of alveolar rhabdomyosarcoma, while PAX7::FOXO1 fusion gene is seen in 10% (Table 1). Abnormal signal patterns of FOXO1 amplification in alveolar rhabdomyosarcoma is a known common phenomenon [1, 6]. 9 (10%, 9/94) cases of alveolar rhabdomyosarcoma showed amplification of 3′ end of the FOXO1 locus in our study. To confirm whether these cases harboured PAX3::FOXO1 or PAX7::FOXO1 fusion gene, FISH with fusion probes and RT-PCR were perform. All of the cases with amplification of FOXO1 locus carried either PAX3::FOXO1 or PAX7::FOXO1 fusion gene. PAX7::FOXO1 fusion gene was detected in 6 cases. 3 cases showed PAX3::FOXO1 fusion gene. These results were consistent with previous reports [14, 15].
The majority of translocations involving EWSR1 gene in mesenchymal neoplasms are balanced translocations. Our results showed that the frequency of abnormal signal patterns of EWSR1 in clear cell sarcoma is very low (2%, 1/61), which is consistent with a previous report [6]. Only one case with an extra copy of EWSR1 locus was found. A novel EWSR1::CREM fusion gene was identified by WGS (Figure 6).
The Ewing sarcoma family of tumours is a group of malignant mesenchymal neoplasms characterized by characteristic EWSR1 gene rearrangement. The most common fusion gene in Ewing sarcoma are EWSR1::FLI1 (85%) followed by EWSR1::ERG (10%) (Table 1). Papp, et al reported one of 93 Ewing sarcoma showed two fusion and one extra red signal [6]. Our results showed that the abnormal signal patterns in Ewing sarcoma were deletions (2%, 8/491) and extra copies (3%, 15/491) of EWSR1 locus. Among the 8 cases with a deletion pattern, EWSR1::FLI1 was detected in 5 cases. EWSR1::ERG was found in 2 cases. The mechanism underpinning the deletion pattern is unknown and further studies are required to investigate the potential causes.
EWSR1::NFATC2 sarcoma is a rare type of sarcoma, first reported by Szuhai et al [16]. This tumour exhibits characteristic clinical and histological features [16–18]. Unlike classical Ewing sarcoma, this tumour displays a characteristic FISH pattern with amplification at the 5′ end of the EWSR1 locus [17, 18] This is due to a genomic rearrangement that fuses the N-terminal transactivation domain of EWSR1 to the C-terminal DNA binding domain of NFATC2, and this fusion is often accompanied by amplification of the 5′ end of the EWSR1 locus. In the literature, this tumour is predominantly located in long bones, nearly half of cases were from the femur [1, 17]. Our results showed 4 of 6 cases were from femur. EWSR1::NFATC2 fusion gene was detected by FISH and NGS in all 6 cases with the amplification of 5′ end of the EWSR1 locus. These results support previous reports [1, 17, 18].
t (7; 16) (q34; p11)FUS::CREB3L2 is the most common chromosome translocation in LGFMS (90%) [19]. 25% of cases harbour supernumerary ring chromosomes 7 and 16 [20, 21]. There are only a few published papers about abnormal signal patterns of break-apart FUS rearrangement in LGFMS [6, 20, 21]. Bartuma et al identified FUS::CREB3L2 fusion gene in supernumerary ring chromosomes in a case of LGFMS [20]. The authors suggested that an unbalanced rearrangement of FUS with supernumerary ring chromosome explained the extra copy of FUS locus. Papp et al reported 4 of 6 cases (67%) LGFMS with two yellow and one or two isolated green signals [6]. However, no further evidence of FUS::CREB3L2 or FUS related fusion gene was investigated by RT-PCR or NGS in these four cases. Our study showed extra copy of 5′ end of the FUS locus as the sole abnormal signal pattern and was detected in 32% (6/19) of cases. FUS::CREB3L2 fusion gene was found in 67% (4/6) of cases by RT-PCR.
Chen et al first reported the deletion of USP6 locus in 1 of 8 cases of nodular fasciitis with MYH9::USP6 fusion gene using FISH and RT-PCR [22]. An extra copy of the USP6 locus was detected in 1 of 6 cases of nodular fasciitis by Papp et al [6]. In our study, 9% (18/209) showed either deletion (16) or an extra copy (2) of USP6 locus. MYH9::USP6 fusion gene was detected in 12 cases by RT-PCR or NGS. A novel FRMD6::USP6 fusion gene was identified in a case with an extra copy of USP6 locus.
Synovial sarcoma harbours a pathognomonic t (X; 18) translocation resulting in either SS18::SSX1, SS18::SSX2 or SS18::SSX4 fusion genes [1]. SS18::SSX1 is the most common fusion gene (90%) followed by SS18::SSX2 (10%). SS18::SSX4 is very rare. Amary et al first displayed deletion signals in 4 of 101 cases of synovial sarcoma by FISH SS18 break-apart probes, thereby highlighting how these unusual patterns can cause uncertainty in the interpretation of FISH results and subsequent challenges in diagnosis [5]. SS18::SSX fusion gene was detected by RT-PCR in all 4 cases. Another study by Papp et al reported 6 of 89 synovial sarcomas showed abnormal signal patterns of the SS18::SSX1 fusion gene using the TriCheck fusion probe and Real-Time PCR [6]. The authors suggested the interpretation of equivocal break-apart FISH results can be validated by FISH using fusion probes and RT-PCR [5]. In our study, abnormal signal patterns were found in 17 cases including 8 cases with deletion and 9 cases with extra copies. SS18::SSX1 (13 cases) and SS18::SSX2 (3 cases) were detected by RT-PCR and NGS in all cases except 1 case without material.
In total, 80 of 1,087 cases showed abnormal signal patterns in bone and soft tissue tumours using break-apart FISH probes. The specific fusion genes were detected by orthogonal methods including FISH with fusion probes, RT-PCR, NGS or WGS in 70 of 77 cases with material available. No specific fusion genes were detected by RT-PCR in 7 cases which could be due to either alternate fusion transcript breakpoints or alternative fusion partner genes that are not covered by primers for the RT-PCR assay.
The deletion signal pattern of the gene does not always have the rearrangement of the gene.
Conclusion
This is a large, retrospective cohort from a specialist bone and soft tissue unit with systematic review of the interpretation of break-apart probe signals in bone and soft tissue tumours. In total, 7% (80/1,087) cases show abnormal break-apart signal patterns. The interpretation of these abnormal signal patterns may be challenging and can lead to false negative results or misdiagnosis. Our retrospective analysis highlighted the frequency of abnormal signal patterns by disease type and demonstrated the need validation testing using orthogonal molecular techniques -e.g. FISH Fusion probes, RT-PCR, targeted RNA sequencing (RNAseq) or Whole Genome Sequencing (WGS).
Statements
Data availability statement
Datasets used in producing this manuscript will be made available upon request to the corresponding authors.
Ethics statement
All data presented for the retrospective audit of cases were generated as part of routine diagnostic pathway. The material for WGS was obtained through the University College London/University College London Hospitals (UCL/UCLH) Biobank for Health and Disease (REC reference 20/YH/0088).
Author contributions
HY, Concept, collection of material and data, FISH analysis, drafting of the manuscript. FB, ER, and EM, FISH analysis. CD, WGS analysis. AF, WGS analysis. NP, Concept, critical revision and final drafting of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. We are grateful to the Edward Showler Foundation for funding of the WGS of for the CCS case and for support of CD and AF. NP holds a Cancer Research UK Career Establishment Award (Ref: RCCCEANov23/100003). CD holds a Sarcoma UK PhD fellowship (SUK09.2022).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
References
1.
The WHO Classification of Tumours Editorial Board, soft tissue and bone tumours (2020) 5th ed (Lyon: IARC).
2.
Nakano K Takahashi S . Translocation-related sarcomas. Int J Mol Sci (2018) 19(12):3784. 10.3390/ijms19123784
3.
Bridge JA . The role of cytogenetics and molecular diagnostics in the diagnosis of soft-tissue tumors. Mod Pathol (2014) 27(Suppl. 1):S80–97. 10.1038/modpathol.2013.179
4.
Oda Y Tsuneyoshi M . Recent advances in the molecular pathology of soft tissue sarcoma: implications for diagnosis, patient prognosis, and molecular target therapy in the future. Cancer Sci (2008) 100(2):200–8. 10.1111/j.1349-7006.2008.01024.x
5.
Amary FM Berisha F Bernardi FDC Herbert A James M Reis-Filho S et al Detection of SS18-SSX fusion transcripts in formalin-fixed paraffin-embedded neoplasms: analysis of conventional RT-PCR, qRT-PCR and dual color FISH as diagnostic tools for synovial sarcoma. Mod Pathol (2007) 20(4):482–96. 10.1038/modpathol.3800761
6.
Papp G Mihaly D Sapi Z . Unusual signal patterns of break-apart FISH probe used in the diagnosis of soft tissue sarcomas. Pathol Oncol Res (2017) 23(4):863–71. 10.1007/s12253-017-0200-z
7.
Vargas AC Selinger C Satgunaseelan L Copper WA Gupta R Stalley P et al Atypical Ewing sarcoma breakpoint region 1 fluorescence in-situ hybridization signal patterns in bone and soft tissue tumours: diagnostic experience with 135 cases. Histopathology (2016) 69(6):1000–11. 10.1111/his.13031
8.
Amary FM Ye H Berisha F Khatri B Forbes G Lehovsky K et al Fibroblastic growth factor receptor 1 amplification in osteosarcoma is associated with poor response to neo-adjuvant chemotherapy. Cancer Med (2014) 3(4):980–7. 10.1002/cam4.268
9.
Chapman B Kirchner R Pantano L Naumenko S Smet MD Beltrame L et al bcbio/bcbio-nextgen, v1.2.9. Zenodo (2021).
10.
Chen X Schulz-Trieglaff O Shaw R Barnes B Schlesinger F Källberg M et al Manta: rapid detection of structural variants and indels for germline and cancer sequencing applications. Bioinformatics (2016) 32(8):1220–2. 10.1093/bioinformatics/btv710
11.
Cameron DL Baber J Shale C Valle-Inclan JE Besselink N van Hoeck A et al GRIDSS2: comprehensive characterisation of somatic structural variation using single breakend variants and structural variant phasing. Genome Biol (2021) 22(1):202. 10.1186/s13059-021-02423-x
12.
Wala JA Bandopadhayay P Greenwald NF O'Rourke R Sharpe T Stewart C et al SvABA: genome-wide detection of structural variants and indels by local assembly. Genome Res (2018) 28(4):581–91. 10.1101/gr.221028.117
13.
Sankar S Lessnick SL . Promiscuous partnerships in Ewing’s sarcoma. Cancer Genet (2011) 204(7):351–65. 10.1016/j.cancergen.2011.07.008
14.
Reichek JL Duan F Smith LM Gustafson DM O’ Connor RS Zhang C et al Genomic and clinical analysis of amplification of the 13q31 chromosomal region in alveolar rhabdomyosarcoma: a report from the Children’s Oncology Group. Clin Cancer Res (2011) 17(6):1463–73. 10.1158/1078-0432.CCR-10-0091
15.
Skapek SX Ferrari A Gupta AA Lupo PJ Butler E Shipley J et al Rhabdomyosarcoma. Nat Rev Dis Primers (2019) 5(1):1. 10.1038/s41572-018-0051-2
16.
Szuhai K Ijszenga M de Jong D Karseladze A Tanke HJ Hogendoorn PCW . The NFATc2 gene is involved in a novel cloned translocation in a Ewing sarcoma variant that couples its function in immunology to oncology. Clin Cancer Res (2009) 15(7):2259–68. 10.1158/1078-0432.CCR-08-2184
17.
Liu L Li L Ding Y Kong F Mo W Ye H et al Report and literature review of four cases of EWSR1::NFATC2 round cell sarcoma. Diagn Pathol (2024) 19:19. 10.1186/s13000-024-01443-y
18.
Watson S Perrin V Guillemot D Reynaud S Coindre JM Karanian M et al Transcriptomic definition of molecular subgroups of small round cell sarcomas. J Pathol (2018) 245(1):29–40. 10.1002/path.5053
19.
Matsuyama A Hisaoka M Shimajiri S Hayashi T Imamura T Ishida T et al Molecular detection of FUS-CREB3L2 fusion transcripts in low-grade fibromyxoid sarcoma using formalin-fixed, paraffin-embedded tissue specimens. Am J Surg Pathol (2006) 30(9):1077–84. 10.1097/01.pas.0000209830.24230.1f
20.
Bartumaa H Möllera E Collina A Domanskib HA Vult Von Steyernc F Mandahla N et al Fusion of the FUS and CREB3L2 genes in a supernumerary ring chromosome in low-grade fibromyxoid sarcoma. Cancer Genet Cytogenet (2010) 199(2):143–6. 10.1016/j.cancergencyto.2010.02.011
21.
Chien YCC Károlyi K Kovács I . Paravertebral low-grade fibromyxoid sarcoma with supernumerary ring chromosome: case report and literature review. Ann Clin Lab Sci (2016) 46(1):90–6.
22.
Chen J Ye X Li Y Wei C Zheng Q Zhong P et al Chromosomal translocation involving USP6 gene in nodular fasciitis. Zhonghua Bing Li Xue Za Zhi (2014) 43(8):533–6. 10.3760/cma.j.issn.0529-5807.2014.08.007
Summary
Keywords
FISH, abnormal signal pattern, break-apart probe, bone and soft tissue tumour, gene rearrangement, translocation, cancer, genomics
Citation
Ye H, Berisha F, Rowles E, Munasinghe E, Davies C, Farswan A and Pillay N (2025) The implications of abnormal signal patterns of break-apart FISH probes used in the diagnosis of bone and soft tissue tumours. Pathol. Oncol. Res. 31:1612142. doi: 10.3389/pore.2025.1612142
Received
31 March 2025
Accepted
03 June 2025
Published
01 July 2025
Volume
31 - 2025
Edited by
Zsolt Orosz, Nuffield Orthopaedic Centre, United Kingdom
Updates
Copyright
© 2025 Ye, Berisha, Rowles, Munasinghe, Davies, Farswan and Pillay.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongtao Ye, hongtao.ye@nhs.net; Nischalan Pillay, n.pillay@ucl.ac.uk
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.