Abstract
Recognition of unusual histological features can augment and hasten a diagnosis but also stimulate ideas about physiological and pathological cellular interactions. Osteoclasts resorb mineralised tissue and therefore can be found at sites of heterotopic bone formation. However, multinucleated giant cells with morphological features of osteoclasts, so called ‘osteoclast-like cells’ can also be encountered in a variety of soft tissue tumours unrelated to ossification and calcification. Prompted by the presence of osteoclast-like cells in undifferentiated pleomorphic sarcoma while undertaking our Artificial Intelligence project for classifying sarcoma, we reviewed the English literature for these cells in soft tissue tumours and we found that this was poorly documented, and much was published before the release of the WHO essential diagnostic criteria in 2020. There were numerous single case reports and small series of a broad range of soft tissue tumours with osteoclast-like cells but only a limited number of diagnoses in which these cells were reported recurrently. We provide a comprehensive update of osteoclast-like cells and mineralisation in soft tissue tumours from the literature. We also present real-world incidence of osteoclast-like cells from selected tumour types in our Whole Slide Image (WSI) library of soft tissue tumours. Assessment of WSI from 1100 different patients showed that osteoclast-like cells were relatively common and under-recognised in nodular fasciitis (18.5 of 200), angiomatoid fibrous histiocytoma (17.5% of 40), undifferentiated pleomorphic sarcoma (15% of 261) and epithelioid sarcoma (9% of 68) while they were never encountered in myxofibrosarcoma (0/250) and clear cell sarcoma of soft tissue (0/80). Awareness of this phenomenon not only helps shape the differential diagnosis but also can be used to stimulate pathobiological questions and to enhance the performance of AI models for classifying disease.
Introduction
The histopathology field has been revolutionised by the major advances in the understanding of the molecular mechanisms of neoplastic disease, and this is reflected in the changes introduced by the recent World Health Organisation classification of tumours series of Blue Books. In the era of complex molecular and genetic analysis, morphology can be easily overlooked. This can only be to the disadvantage of a great part of the world where access to advanced ancillary testing is, at best, limited, and where morphology and restricted use of immunohistochemistry remains the cornerstone in surgical pathology.
While working on our Artificial Intelligence (AI) project for classifying sarcoma (AI-SCOPE: Artificial Intelligence for SarComa Outcome PrEdiction [1]), we noted that the incidence of osteoclast-like cell was relatively common in several tumours. We identified numerous case reports, but an overview of the subject was not available. This prompted us to review how often osteoclast-like cells and mineralisation (ossification and calcification) were described in soft tissue tumours in the recent WHO classification of tumours series. We also reviewed digitised whole slide images (WSI) of specific diagnoses as part of AI-SCOPE to assess the incidence of these features in soft tissue tumours employing standards of classification based on current WHO Books.
Osteoclasts are haematopoietic cells originating from myeloid progenitors under the stimulation of key factors such as CSF-1 [2] and receptor activator of nuclear factor-kB ligand (RANKL) [3–5]. Their primary function is to maintain a healthy skeleton through bone reabsorption brought about by a tightly regulated physiological process involving interplay between several molecules, ensuring appropriate recruitment to sites requiring bone replacement. Disruption of these processes manifests most commonly as unregulated osteolysis of the skeleton and is seen in common diseases such as osteomyelitis, osteoporosis, and metastatic neoplasms to bone [6] and rarely in primary bone tumours [7, 8] and less commonly in reduced osteoclast numbers and or function, as in osteopetrosis [9].
Osteoclasts in extra-skeletal sites are an abnormal finding, they occur commonly in combination with soft tissue calcification and/or ectopic bone formation, which comes about by the reactivation of bone-forming programmes involving the recruitment of local stem cells to form bone and cartilage, remodelling of the bone through osteoclast activity and the formation of mature bone [10].
Heterotopic bone is commonly caused by trauma and ischaemia, resulting in dystrophic calcification, which can be the forerunner of ossification. This process is not uncommonly seen in tumours, but it is a non-specific finding and can happen in virtually all neoplasms. In contrast, mineralisation is an essential criterion for some neoplasms including extra-skeletal osteosarcoma, and calcifying aponeurotic fibroma, amongst others [11, 12]. Autoimmune disease can also account for ectopic mineralisation, exemplified by calcinosis cutis [6, 12, 13]. It has long been recognised that a wide variety of tumours, including many types of carcinoma particularly pancreas, breast and others [14, 15], and also uterine smooth muscle tumours [16], harbour osteoclast-like giant cells generally in the absence of mineralisation. The term osteoclast-like cell is preferred to ‘osteoclast’ as it can be challenging and sometimes impossible to distinguish osteoclasts from the other types of multinucleate giant cells because of their overlapping morphological features; these include so-called foreign body, Tuton and Langhans giant cells (Figure 1). However, osteoclasts uniquely have the ability to resorb bone [17] and historically, this function was employed to define osteoclasts in an experimental setting [17] and was used to establish that the multinucleate giant cells in tenosynovial giant cell tumours (previously known as pigmented villonodular synovitis [18]), pilar tumour of the scalp [19] and giant cell tumour of tendon sheath [20] and in an undifferentiated pleomorphic sarcoma, previously known as malignant fibrous histiocytoma [21], were accurately classified as osteoclasts [22]. Previous studies, summarised in an overview [23] have shown that osteoclasts can also be distinguished from other multinucleate giant cells by the expression of the calcitonin receptor, the vitronectin receptor and tartrate-resistant acid phosphatase and the absence of HLA-DR. However, it is no longer considered valuable to undertake such experimental and immunohistochemistry profiling in a diagnostic setting. From a practical diagnostic perspective, the classification of an ‘osteoclast-rich tumour’ is based on the presence of a large number of such cells and, therefore is not considered a major challenge in distinguishing osteoclasts from other multinucleate cells.
FIGURE 1
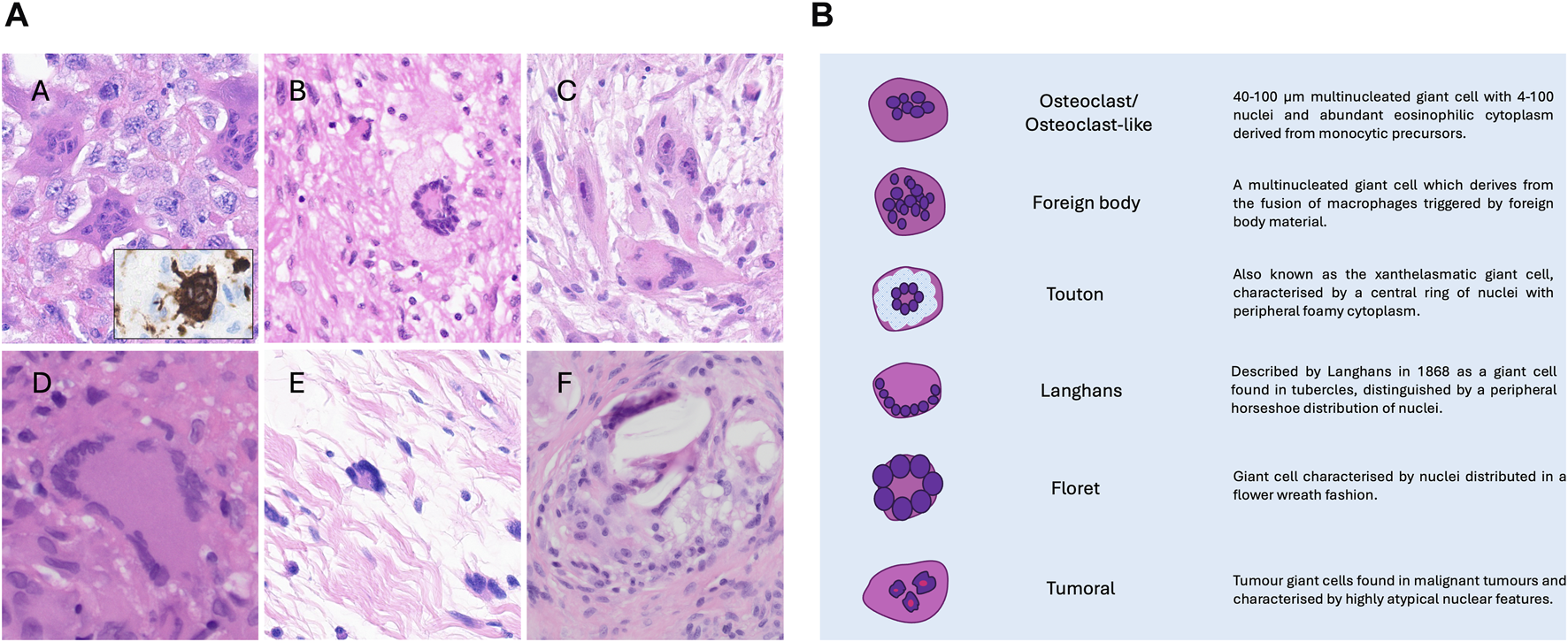
(A) Photomicrographs of hematoxylin and eosin-stained sections showing different kinds of multinucleated giant cells. Osteoclast-like giant cells in undifferentiated pleomorphic sarcoma. CD68 immunostain highlights the dendritic processes typical of those cells (A); A touton giant cell in myxofibrosarcoma (B); tumour multinucleate giant cells in myxofibrosarcoma exhibiting atypical pleomorphic nuclei (C); Langhans-type giant cells in a sarcoidosis granuloma (D); floret multinucleated cell in a pleomorphic lipoma (E); foreign body giant cells (F). Cases from the AI Scope library. (B) Schematic representation of giant cells.
The mechanism explaining the presence of osteoclast-like cells in tumours in the absence of mineralisation is generally unknown. Although RANKL is an important molecule in osteoclast recruitment [24] there is no strong evidence that its expression, in concentration or duration, is the cause of the osteoclast-like cells in these tumours. However, a fusion gene involving CSF-1, resulting in its elevated expression, is found in tenosynovial giant cell tumours explains the presence of osteoclasts in these tumours [25]. More recently, giant cell tumours of soft tissue have been found to harbour a HMGA2::NCOR2 fusion gene, although it is unknown how this mediates osteoclast-like cell recruitment [26, 27].
Here, using the presence of osteoclast-like cells and mineralisation in soft tissue tumours as an exemplar, we highlight the value of detailing morphological features in tumour pathology. Such information would benefit the majority of pathologists around the world who have at best limited access to advanced technologies, including immunohistochemistry and next-generation sequencing, in delivering their clinical practice. In the context of AI, which is rapidly being introduced into surgical pathology, morphology is far from obsolete because AI algorithms for disease classification are mainly trained on haematoxylin and eosin-stained digitalised slides. Although large pathology foundation models are self-supervising, thereby overcoming the need for annotation of images by pathologists [28–30], training models for classifying rare diseases, such as sarcoma and its mimics, will likely require annotation by pathologists for some time to come [31]. This underscores the importance of the identification of morphological features as described in the manuscript. Lastly, appreciation of histological features both stimulates and allows the analysis of mechanisms of disease to be investigated.
Materials and methods
Literature revision
A list of soft tissue tumours (Supplementary Table S1) was obtained from the latest editions of the WHO Classification of Tumours series of books including Soft tissue and bone tumours (2020), Digestive system tumours (2019), Skin tumours (beta online version) Breast tumours (2019), Head and neck tumours (2023), Eye and orbit tumours (beta online version), Thoracic tumours (2021), Urinary and male genital tumours (2024), Paediatric tumours (2022) and Haematolymphoid tumours (2024) [32–41]. In addition, we included three emerging entities [42–44] not found in the WHO books, which are documented as containing osteoclasts of which we are aware from our diagnostic practice, published literature and data accrued from the North Thames Genome Laboratory Hub. Mesenchymal tumours originating from bone and uterus were not included.
The presence of “osteoclast-like cells” and mineralisation, including ossification and calcification, was sought in the histopathology description in the WHO books listed above and recorded (Supplementary Table S1). For each listed diagnosis, we interrogated the English literature using PubMed and Google Scholar for records of osteoclast-like cells and mineralisation in soft tissue tumours.
Case review and data collection
We reviewed Whole Slide Images (WSI) from cases from England and Wales included in our AI SCOPE library (one or two slides per case) built with tumours classified according to the essential criteria in the current WHO Books along with at least one confirmatory ancillary testing, such as immunohistochemistry, fluorescence in situ hybridisation (FISH), or next-generation sequencing (NGS), for example, detection of a USP6 rearrangement in nodular fasciitis. Additional diagnoses were also reviewed for reasons described in the Results section.
Recognising the challenge in distinguishing osteoclasts from different forms of multinucleate cells, we have employed the term ‘osteoclast-like’ giant cells in the tumours studied. To mitigate further misclassification, clusters of such cells were required to be identified within a tumour. Figure 1 shows the different forms of multinucleate cells and describes their distinguishing features.
Ethical approval was given for undertaking the study “An Artificial Intelligence (AI) solution for diagnosing, prognosticating as well as predicting outcome of sarcomas and their mimics: a multi-centre study.” IRAS project ID: 328987 Protocol number: EDGE 161548. REC reference: 23/NI/0166. Sponsor University College London has been approved by HRA and Health and Care Research Wales (HCRW) (14th December 2023) and by Health and Social Care Research Ethics Committee B (HSC REC B) Office for Research Ethics Committees Northern Ireland (ORECNI) Lissue Industrial Estate West, 5 Rathdown Walk, LISBURN, BT28 2RF. REC reference: 23/NI/0166, Protocol number: EDGE 161548, IRAS project ID: 328987 (December 2023).
Results
Interrogation of the WHO Books for the presence of osteoclast-like cells in soft tissue tumours revealed 14 diagnoses. An additional 29 entities were extracted from the literature, including three recently described diagnoses [42–44], giving a total of 43 of 164 tumours (Supplementary Table S1).
Mineralisation in soft tissue tumours
Next, we performed a literature search for mineralisation in soft tissue tumours. This revealed that 69 of the 164 tumours identified above contained mineralisation, 30 of which were also reported to harbour osteoclasts (Supplementary Table S1). However, in most of these lesions, the amount of mineralisation was limited and present infrequently and importantly, the feature was not useful for prompting a diagnosis. Conversely, mineralisation is an essential diagnostic requirement for some soft tissue tumours, for example, extra-skeletal osteosarcoma in which osteoclast-like cells can frequently be present [45] (Table 1). Finally, the search revealed sarcomas in which mineralisation was not an infrequent occurrence, and in which osteoclast-like cells have not been reported, but where it is a useful diagnostic hint for both pathologists and radiologists. Synovial sarcoma and ossifying fibromyxoid tumour are good examples, with mineralisation reported in 30% and 67% of cases, respectively, although this is old literature and was not based on molecular classification [46, 48]. Less recognised mineralisation occurs in low grade fibromyxoid sarcoma [49] (Figure 2). Other examples are listed in Table 1. Figure 3 highlights different types of mineralisation that are found in soft tissue lesions.
TABLE 1
| Diagnosis | Mineralisation |
|---|---|
| a Calcifying aponeurotic fibroma | Essential criteria |
| a Extra-skeletal osteosarcoma (and other sarcomas with osteosarcomatous differentiation e.g. malignant peripheral nerve sheath tumour and dedifferentiated liposarcoma) | Essential criteria |
| a Phosphaturic mesenchymal tumour | Essential criteria |
| a Myositis ossificans/fibro-osseous pseudo-tumour of the fingers | Essential criteria |
| a Soft tissue chondroma | Common (% n/a) |
| Ossifying fibromyxoid tumour | 67% [46] |
| Malignant melanotic nerve sheath tumour | 40% [47] |
| Synovial Sarcoma | 30% [48] |
Soft tissue tumours in which mineralisation (ossification and or calcification) represents a common feature and or is diagnostically useful.
In which osteoclast-like cells are commonly seen.
FIGURE 2
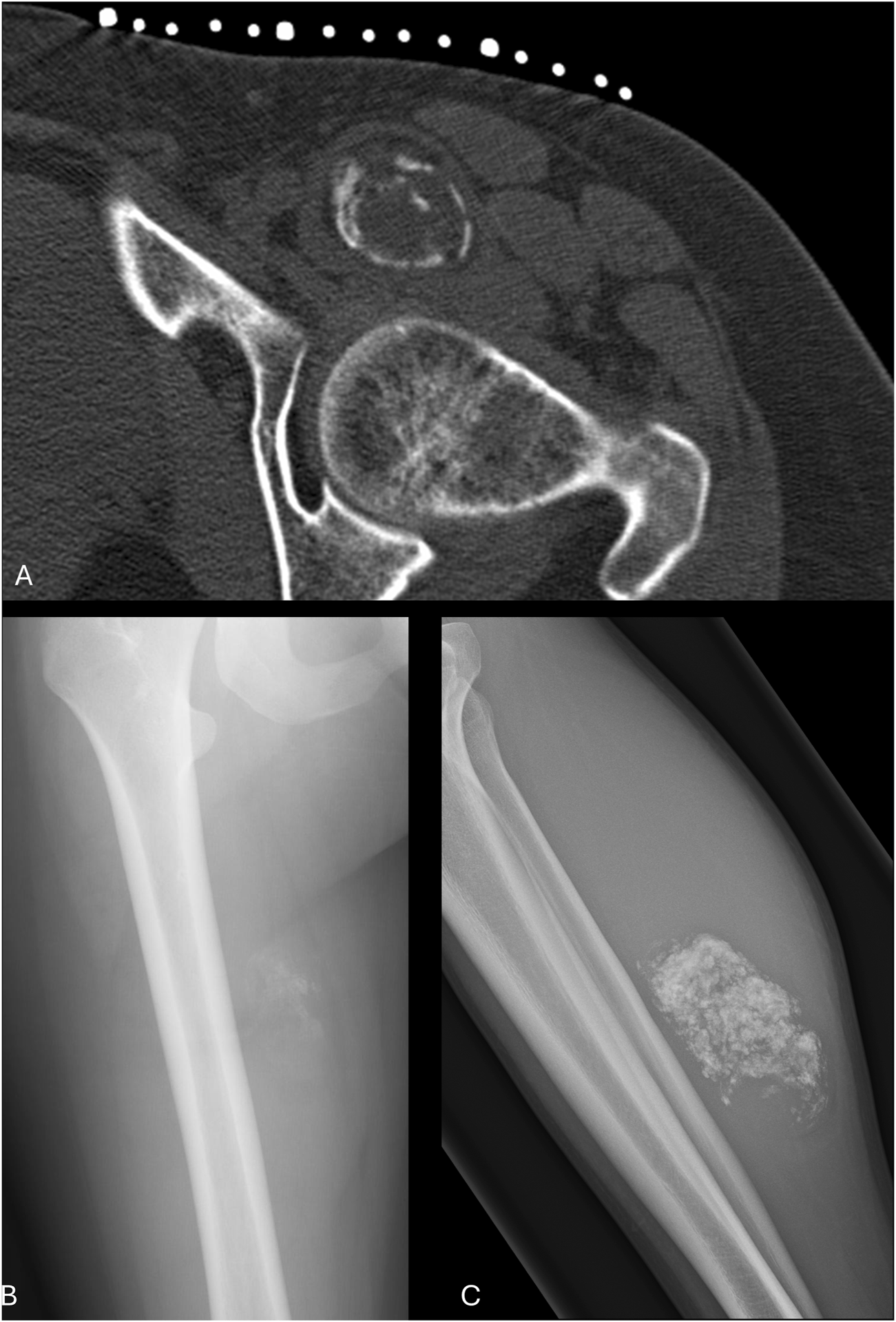
Radiology of calcified soft tissue masses. Axial CT shows an ossifying fibromyxoid tumour anterior to the left hip with a thin, incomplete bone margin (A); AP radiograph of the right femur shows faint amorphous mineralisation projected medial to the bone in a synovial sarcoma (B); lateral radiograph of the right tibia and fibula shows dense mineralisation in the posterior calf in a low-grade fibromyxoid sarcoma (C). Each case shown harboured the relevant recurrent fusion gene characteristic of the tumour type namely PHF1::HCFC1, SS18-SSX and FUS::CREB3L2.
FIGURE 3
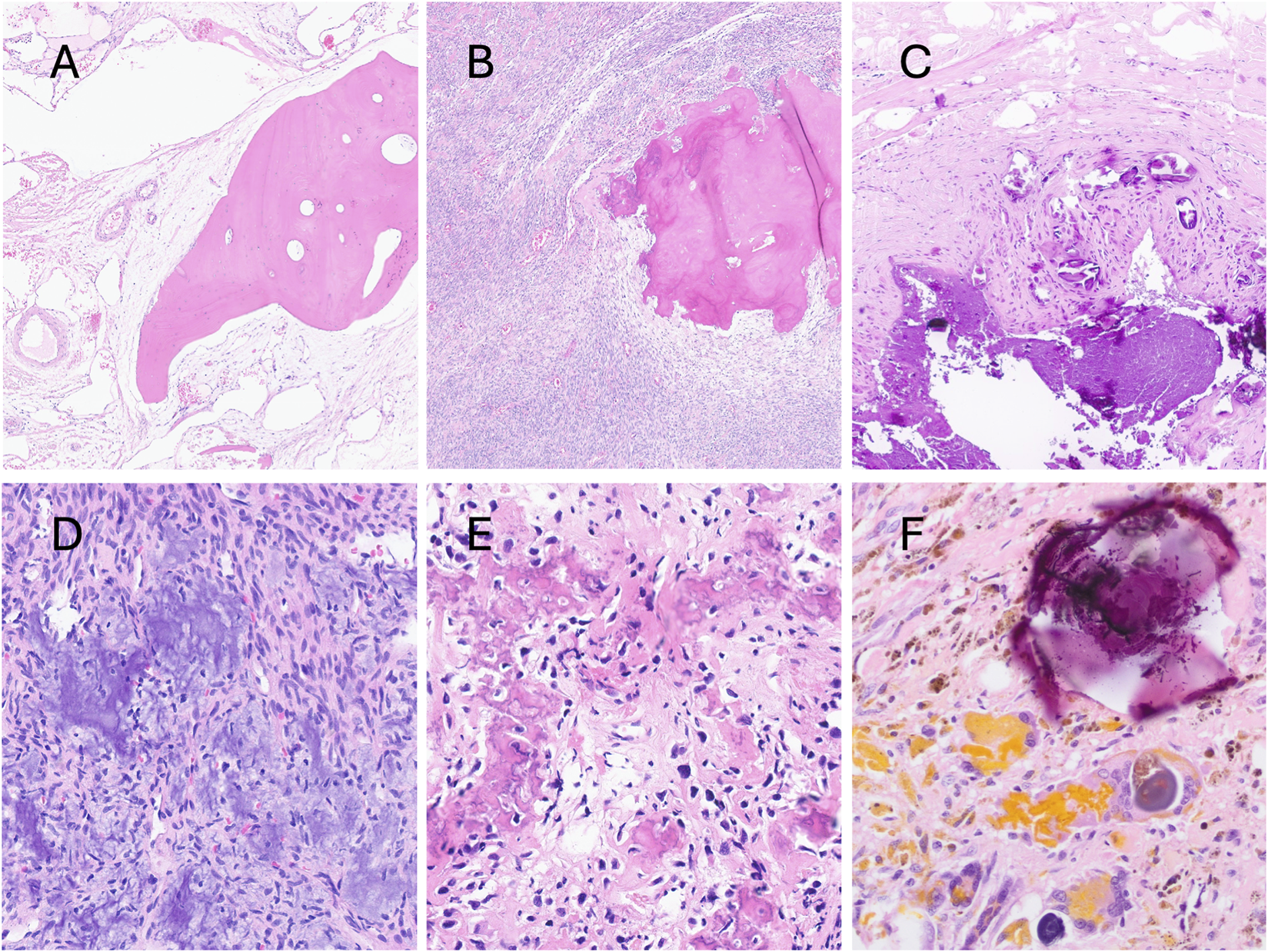
Photomicrographs of hematoxylin and eosin-stained sections of soft tissue lesions exhibiting different forms of mineralisation. Metaplastic mature compact bone in an intramuscular vascular malformation (A). Calcification in synovial sarcoma (B); tumoral calcinosis (C); grungy calcifications in phosphaturic mesenchymal tumour (D); irregular bone deposition in extraskeletal osteosarcoma (E); psammoma bodies in malignant melanotic nerve sheath tumour (F).
Osteoclasts in soft tissue tumours
Of the 43 tumour types with osteoclast-like cells identified in the WHO Books and the literature most have only been reported as single case reports or small series (Supplementary Table S1). We found only six tumour types that were reported to frequently contain ectopic osteoclasts and in which their distribution is not restricted to the site where bone or calcified material is deposited (Table 2). Giant cell tumour of soft parts, for which osteoclast-like giant cells are an essential diagnostic requirement, but where focal bone deposition is reported in 40.1% of cases [55], tenosynovial giant cell tumours, which harbour osteoclasts in 50%–100% of cases [52, 53], in 63% of plexiform fibrohistiocytic tumour [54] and 50% of Gastrointestinal clear cell sarcoma/malignant gastrointestinal neuroectodermal tumour [33]. Furthermore, osteoclast-like cells are reported to be found consistently, but less frequently, in 24% of 25 cases of angiomatoid fibrous histiocytoma [51], and in 10% of nodular fasciitis in the largest series (272 cases) published so far [50]. However, despite the authors casting doubt on whether these cells were true osteoclasts, on review of their published photomicrographs, we are confident that the multinucleated cells represented osteoclast-like cells. It is also reassuring to find that Montgomery et al. had already recognised osteoclast-like cells in nodular fasciitis [56]. It is noteworthy that both reports were published prior to the discovery of USP6 being rearranged recurrently in nodular fasciitis. Likewise, Maqbool et al. [51] published their findings on osteoclasts in angiomatoid fibrous histiocytomas, but information on the presence of aEWSR1 rearrangement was not provided.
TABLE 2
| Diagnosis | Number of cases reviewed | Number of cases containing osteoclast-like cells (%) | Previous reports of osteoclast-like cells: Number studied (%) |
|---|---|---|---|
| Nodular fasciitisa | 200 | 36 (18) | (10) [50] |
| Undifferentiated sarcomaa pleomorphic and spindle cell sarcoma | 261 | 39 (15) | Case reportsb |
| Myxofibrosarcoma | 250 | 0 | Not reported |
| Epithelioid sarcomaa | 68 | 6 (9) | Case reportsb |
| Leiomyosarcoma (non-uterine) | 201 | 5 (2.5) | Case reportsb |
| Clear cell sarcoma | 80 | 0 | Not reported |
| Angiomatoid fibrous histiocytoma | 40 | 7 (17.5) | (24) [51] |
| Tenosynovial giant cell tumour | Not reviewed as osteoclasts seen in vast majority of cases | (50–100) [52, 53] | |
| Giant cell tumour of soft partsa | Not reviewed as osteoclasts essential for the diagnosis | (100) | |
| Plexiform fibrohistiocytic tumour | Not reviewed (insufficient cases) | (63) [54] | |
| Gastrointestinal clear cell sarcoma | Not reviewed (insufficient cases) | (50) [33] | |
In-house review of whole slide images of soft tissue tumours for osteoclast-like cells.
Reported to have mineralisation uncommonly and generally in limited amounts.
In house internal WSIs library review
We next conducted an internal review of our WSI library for our Sarcoma AI project for some those entities identified in the literature to contain ectopic osteoclasts, generally in the absence of mineralisation, and listed in Table 2. In addition to the six diagnoses for which there is strong published evidence for osteoclast-like cells, we extended our review of WSI to an additional four diagnoses based on our observations (unpublished data) (Table 2).
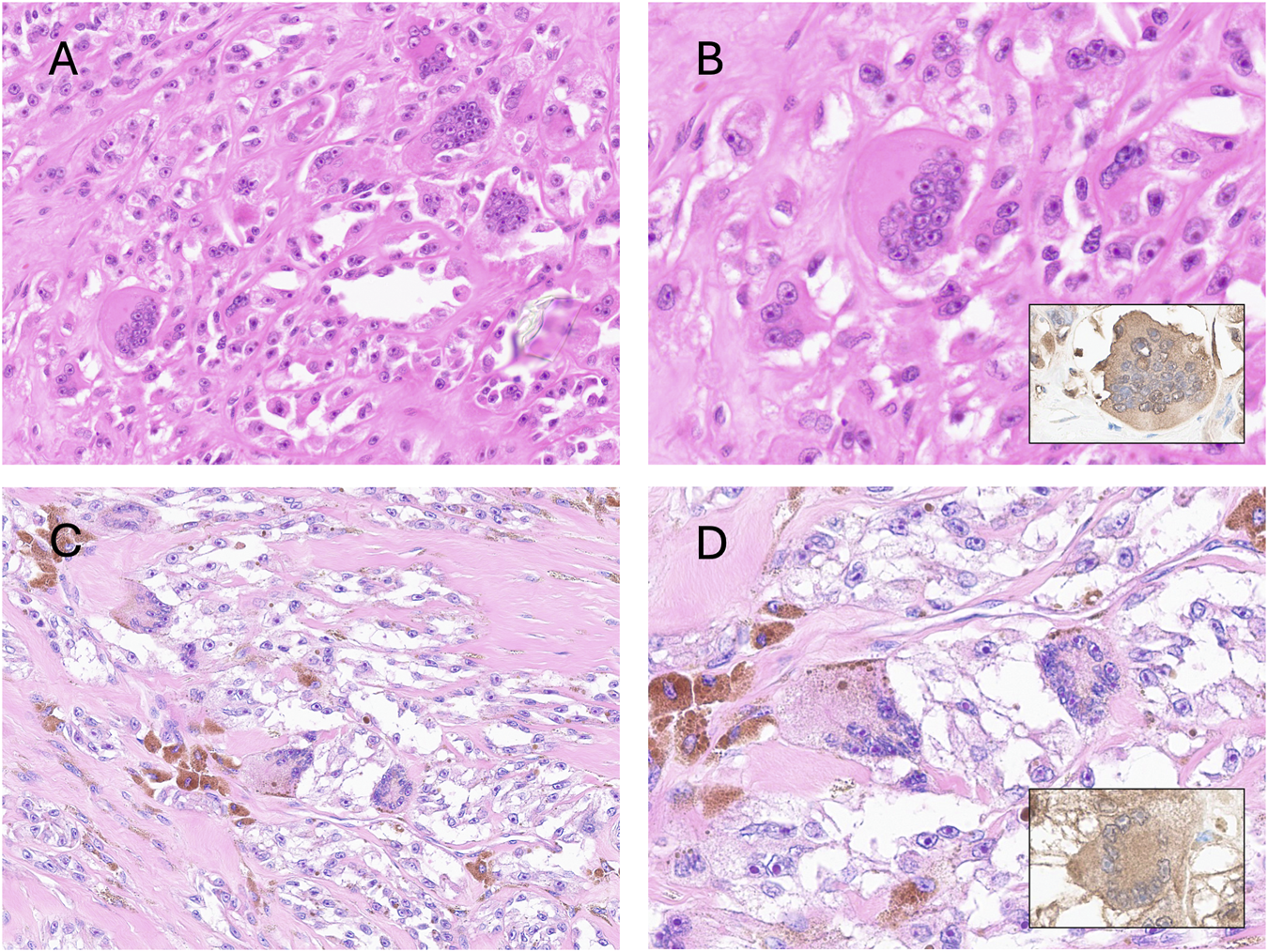
The number, size and distribution of osteoclasts-like giant cells varied considerably between tumours but in general, they occurred scattered irregularly in clusters but sometimes formed sheets or occurred as individual cells. The number of nuclei in the osteoclasts also varied considerably (Figure 4).
FIGURE 4
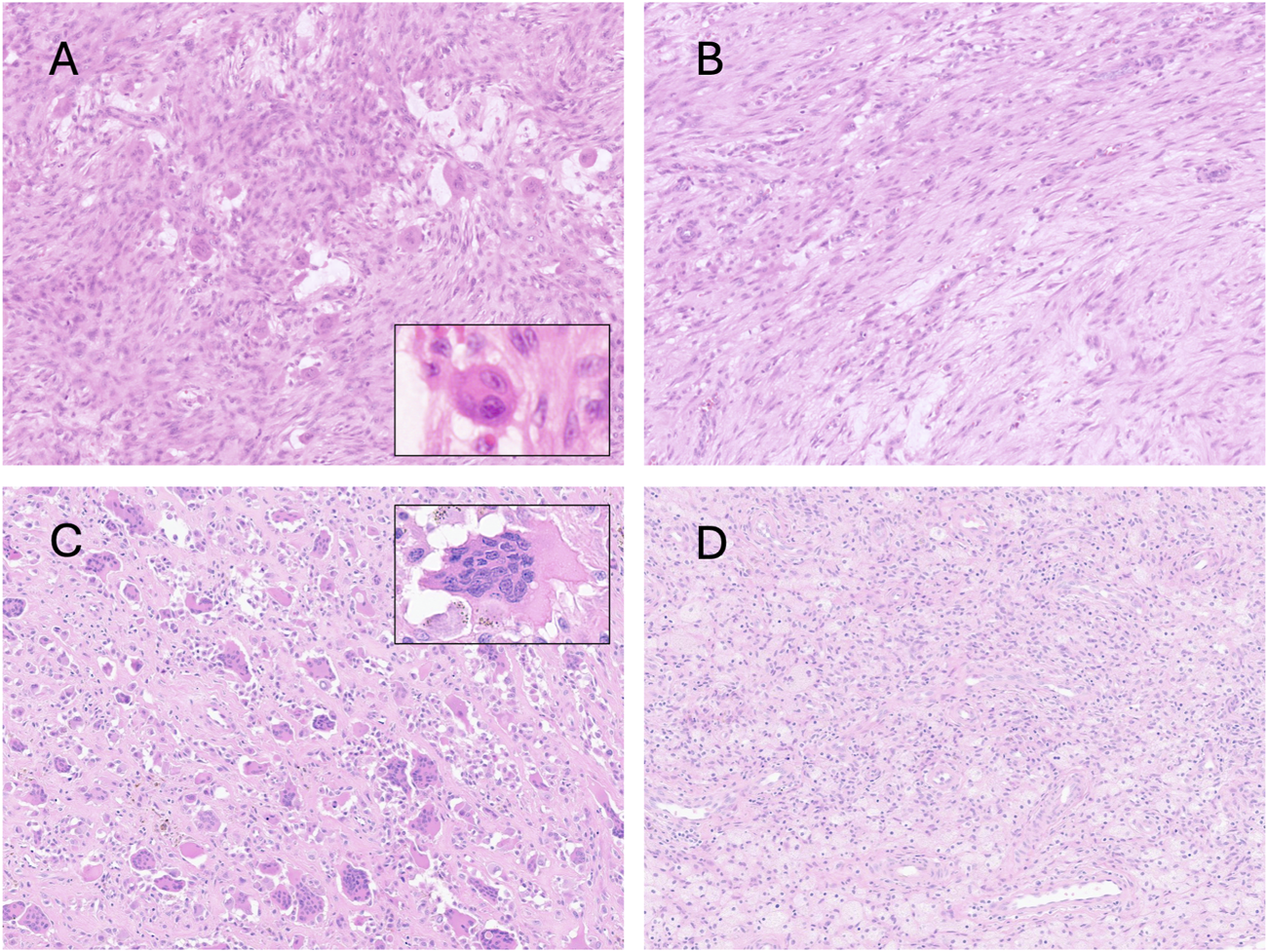
Photomicrographs of hematoxylin and eosin-stained slides showing variability in the distribution of osteoclast-like cells. Zonal variability in the same case of nodular fasciitis (A,B); Two cases of tenosynovial giant cell tumour, with (C) and without (D) osteoclast-like cells. The insets show variability between the size of the cells and the number of nuclei can vary considerably.
Table 2 shows the tumour types in which we identified the frequency of osteoclast-like cells compared with previous reports. We have added to the literature by showing that 15% of undifferentiated sarcomas contained osteoclast-like cells. We also reviewed WSI from 250 myxofibrosarcomas, as these tumours often lose their myxoid matrix as the tumour evolves, and myxoid-poor areas can be difficult to distinguish from undifferentiated sarcomas histologically and genomically [57]. It was noteworthy that osteoclasts were not identified in any of the reviewed cases. However, large Touton-type giant cells were noted in these and some other tumour type, in addition to tumour giant cells (Figure 1aB,C).
Osteoclast-like cells are described as a prevalent feature of clear cell sarcoma of the gastrointestinal tract/malignant neuroectodermal tumours [58]. We were unable to provide information as to how commonly this is seen, as our image library contains insufficient cases. However, we reviewed 80 WSIs of clear cell sarcoma of soft tissue, a tumour with strong morphological and molecular similarities to its gastrointestinal counterpart and failed to identify osteoclast-like cells therein. Interestingly, tumour giant cells, which could be mistaken for osteoclast-like giant cells, were frequently encountered. These generally exhibit a peripheral nuclear distribution, but the cytoplasmic features are comparable to those of adjacent tumour cells (Figure 5).
FIGURE 5
Photomicrographs of hematoxylin and eosin-stained sections showing two cases of clear cell sarcoma of tendons and aponeurosis. The top row case (A,B) contains tumoral giant cells with morphological features overlapping those of osteoclasts. The second case (C,D) contains tumour giant cells with wreath-like peripheral distribution, and melanin pigment is noted in the cytoplasm. The insets show immunoreactivity for S100.
Discussion
Here we present a comprehensive overview of osteoclast-like cells and mineralisation in soft tissue tumours. Although not specific for any entity, awareness of these unusual features can help pathologists hone down on a differential diagnosis, reduce the number of molecular tests and render a definitive diagnosis more rapidly. At the outset, our focus was to catalogue tumours in which osteoclast-like cells occurred outside the skeletal system, such as in undifferentiated sarcomas, as we found it intriguing as to why this might occur.
However, we quickly realised that a significant number of soft tissue tumours are partly mineralised and therefore osteoclast-like cells would also be found in these lesions, as this is the physiological microenvironment to which they are recruited. Such examples include extra-skeletal osteosarcoma, dedifferentiated liposarcoma with osteosarcomatous differentiation and calcifying aponeurotic fibroma. Somewhat misleading from the nomenclature, only 67% of ossifying fibromyxoid tumours contain mineralisation [46]. Ultimately, we identified nine tumour types in which osteoclast-like cells appear relatively commonly in which they are not spatially related to mineralised tissue.
For pathologists to use histological features optimally for guiding clinical management requires that they interpret them in the clinical context. However, today, pathologists can often resolve a differential diagnosis by using molecular tests which screen for a wide range of alterations and provide a pathognomonic alteration. However, globally, most pathologists have limited access to sophisticated investigations and still rely on microscopy to make diagnoses and guide treatment. This highlights the importance of awareness of morphological features. As the WHO Classification of Tumours series of books represent a cornerstone for supporting pathologists world-wide in providing a diagnostic service, it remains important to provide diagnostically useful histological descriptions.
The value of recognising microscopic features but also reflecting on how they inform a diagnosis, has long provided insight into the pathogenesis of disease and has been the initiating stimulus that has resulted in the development of personalised treatment. For instance, recognition by pathologists of a gastrointestinal tract tumour that was neither of smooth muscle nor of nerve sheath origin and that is now recognised as “gastrointestinal stromal tumour” and is now treated with c-kit inhibitors has changed the clinical management and outcome of this disease [59]. Involving pathologists in discovery research has also played a crucial role in translational research and targeted treatments [5]; David Lacey, a pathologist with knowledge of bone disease and osteoclast biology, and his co-authors, recognised the importance of the profound osteopetrosis found in transgenic mice generated by the hepatic expression of an orphan protein identified while undertaking a sequencing study involving fetal rat intestine. They theorised that this molecule blocked osteoclast formation and the experiments led to the identification of Osteoprotegerin [60] and subsequently to the discovery of RANKL [55], and ultimately to the development of denosumab [61].
Although the cellular interactions at a molecular level involved in bone biology have changed dramatically since the discovery of RANKL [62], there is still much to learn. Research continues to reveal genetic alterations that disrupt the physiological process, including H3F3A mutations in giant cell tumour of bone [63], and germline mutations in the zinc finger protein 687 (ZNF687) and PFN1 genes both resulting in multiple giant cell tumour-like lesions arising on a background of Pagetic bone disease [64–66]. However, the mechanisms by which these alterations drive disease is not understood. The availability of spatial transcriptomics now permits these questions to be addressed in an unprecedented manner by allowing the cellular interactions in tumours and their spatial relationships to be studied. This technology should allow identification of molecules involved in ectopic osteoclast recruitment in soft tissue tumours and provide new knowledge of both the physiological and pathological processes in bone and possibly deliver opportunities for the development of novel therapies.
There are limitations of the study: we only reviewed a maximum of two slides per case for the presence of osteoclasts. This is likely to have resulted in an under-estimate of the incidence of osteoclast-like cells in tumours analysed. Despite efforts to ensure that our literature searches were thorough, it is possible that we have overlooked some evidence. Review of the literature also demonstrated that some of the publications available on the subjects discussed are old, and employ historic nomenclature, such as malignant fibrous histiocytoma [21] and pigmented villonodular synovitis [18]. Furthermore, in some instances, the only literature available was prior or in the absence of robust molecular markers. Specifically, the incidence of mineralisation in synovial sarcoma is 30 years old and is based on radiological images [48].
The speed at which new information is being generated in all aspects of pathology is unprecedented. The challenge is how best to exploit it and use it safely. Harnessing artificial intelligence is likely to be the solution, but this will only be achieved safely with significant input from pathologists who appreciate and value morphological features [31].
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was given for undertaking the study “An Artificial Intelligence (AI) solution for diagnosing, prognosticating as well as predicting outcome of sarcomas and their mimics: a multi-centre study.” IRAS project ID: 328987 Protocol number: EDGE 161548. REC reference: 23/NI/0166. Sponsor University College London has been approved by HRA and Health and Care Research Wales (HCRW) (December 14th 2023) and by Health and Social Care Research Ethics Committee B (HSC REC B) Office for Research Ethics Committees Northern Ireland (ORECNI) Lissue Industrial Estate West, 5 Rathdown Walk, LISBURN, BT28 2RF. REC reference: 23/NI/0166, Protocol number: EDGE 161548, IRAS project ID: 328987 (December 2023). The study did not directly include human participants. Only fully anonymised pathology images were included in the study. Therefore written informed consent from patients/guardians/next of kin was not required.
Author contributions
AA selected cases, reviewed cases for presence of osteoclasts, literature review; CS analysed the data, wrote the paper, literature review; FO scanned images, collected data and anonymised the data; AT scanned images, collected data and anonymised the data; RT reviewed diagnoses; FA reviewed diagnoses; PO’D contributed the medical imaging and legends and critically reviewed the paper; AMF conceived the concept, wrote the paper. All authors contributed substantially to the MS, read and approved the final version.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This project was supported by EPSRC UKRI Funding services Grant Ref: EP/Y020030/, Sarcoma UK (SUKRI.2023), BCRT (BCRT/5717) and the Royal National Orthopaedic Hospital Research. AK was supported by the Hashemite University, Jordan. AMF is supported by the National Institute for Health Research, UCLH Biomedical Research Centre, and the CRUK Experimental Cancer Centre.
Acknowledgments
We thank the UCL/UCLH Biobank for Studying Health and Disease for the provision of human tissue samples and clinical data and are grateful to the Biobank Team at the RNOH and all healthcare workers who cared for the patients without whose input this work would not have been possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.por-journal.com/articles/10.3389/pore.2025.1612175/full#supplementary-material
References
1.
Flanagan A . Artificial intelligence project for improved sarcoma diagnoses for patient benefit. (2024). 10.1186/ISRCTN51713388
2.
Mun SH Park PSU Park-Min K-H . The M-CSF receptor in osteoclasts and beyond. Exp Mol Med (2020) 52:1239–54. 10.1038/s12276-020-0484-z
3.
Martin TJ . Reflecting on some discoveries of 40 years and their outcomes. J Bone Mineral Res (2017) 32:1971–6. 10.1002/jbmr.3282
4.
Durdan MM Azaria RD Weivoda MM . Novel insights into the coupling of osteoclasts and resorption to bone formation. Semin Cell and Developmental Biol (2022) 123:4–13. 10.1016/j.semcdb.2021.10.008
5.
Martin TJ . Historically significant events in the discovery of RANK/RANKL/OPG. World J Orthop (2013) 4:186–97. 10.5312/wjo.v4.i4.186
6.
Lerner UH . Osteoclasts in health and disease. Pediatr Endocrinol Rev (2019) 17:84–99. 10.17458/per.vol17.2019.l.osteoclastshealthdisease
7.
Amary F Berisha F Ye H Gupta M Gutteridge A Baumhoer D et al H3F3A (histone 3.3) G34W immunohistochemistry: a reliable marker defining benign and malignant giant cell tumor of bone. Am J Surg Pathol (2017) 41:1059–68. 10.1097/PAS.0000000000000859
8.
Cottone L Ligammari L Lee H-M Knowles HJ Henderson S Bianco S et al Aberrant paracrine signalling for bone remodelling underlies the mutant histone-driven giant cell tumour of bone. Cell Death Differ (2022) 29:2459–71. 10.1038/s41418-022-01031-x
9.
Funck-Brentano T Zillikens MC Clunie G Siggelkow H Appelman-Dijkstra NM Cohen-Solal M . Osteopetrosis and related osteoclast disorders in adults: a review and knowledge gaps on behalf of the European calcified tissue society and ERN BOND. Eur J Med Genet (2024) 69:104936. 10.1016/j.ejmg.2024.104936
10.
Hwang CD Pagani CA Nunez JH Cherief M Qin Q Gomez-Salazar M et al Contemporary perspectives on heterotopic ossification. JCI Insight (2022) 7:e158996. 10.1172/jci.insight.158996
11.
Puls F Hofvander J Magnusson L Nilsson J Haywood E Sumathi VP et al FN1-EGF gene fusions are recurrent in calcifying aponeurotic fibroma. J Pathol (2016) 238:502–7. 10.1002/path.4683
12.
Sajjadi E Gaudioso G Terrasi A Boggio F Venetis K Ivanova M et al Osteoclast-like stromal giant cells in breast cancer likely belong to the spectrum of immunosuppressive tumor-associated macrophages. Front Mol Biosci (2022) 9:894247. 10.3389/fmolb.2022.894247
13.
Reiter N El-Shabrawi L Leinweber B Berghold A Aberer E . Calcinosis cutis: part I. Diagnostic pathway. J Am Acad Dermatol (2011) 65(1–12):1–12. 10.1016/j.jaad.2010.08.038
14.
Demetter P Maréchal R Puleo F Delhaye M Debroux S Charara F et al Undifferentiated pancreatic carcinoma with osteoclast-like giant cells: what do we know So far? Front Oncol (2021) 11:630086. 10.3389/fonc.2021.630086
15.
Cyrta J Benoist C Masliah-Planchon J Vieira AF Pierron G Fuhrmann L et al Breast carcinomas with osteoclast-like giant cells: a comprehensive clinico-pathological and molecular portrait and evidence of RANK-L expression. Mod Pathol (2022) 35:1624–35. 10.1038/s41379-022-01112-9
16.
Aru A Norup P Bjerregaard B Andreasson B Horn T . Osteoclast-like giant cells in leiomyomatous tumors of the uterus. A case report and review of the literature. Acta Obstet Gynecol Scand (2001) 80:371–4. 10.1080/j.1600-0412.2001.080004371.x
17.
Chambers TJ . The birth of the osteoclast. Ann N Y Acad Sci (2010) 1192:19–26. 10.1111/j.1749-6632.2009.05224.x
18.
Neale SD Kristelly R Gundle R Quinn JM Athanasou NA . Giant cells in pigmented villo nodular synovitis express an osteoclast phenotype. J Clin Pathol (1997) 50:605–8. 10.1136/jcp.50.7.605
19.
Afhanasou NA Quinrz JM . Bone resorption by macrophage polykaryons of a pilar tumor of scalp. Cancer (1992) 70:469–75. 10.1002/1097-0142(19920715)70:2<469::AID-CNCR2820700215>3.0.CO;2-0
20.
Athanasou N Quinn J Ferguson D McGee J . Bone resorption by macrophage polykaryons of giant cell tumour of tendon sheath. Br J Cancer (1991) 63:527–33. 10.1038/bjc.1991.125
21.
Fletcher CD . Pleomorphic malignant fibrous histiocytoma: fact or fiction? A critical reappraisal based on 159 tumors diagnosed as pleomorphic sarcoma. Am J Surg Pathol (1992) 16:213–28.
22.
Flanagan AM Chambers TJ . Osteoclasts are present in the giant cell variant of malignant fibrous histiocytoma. The J Pathol (1989) 159:53–7. 10.1002/path.1711590112
23.
Maggiani F Forsyth R Hogendoorn PCW Krenacs T Athanasou NA . The immunophenotype of osteoclasts and macrophage polykaryons. J Clin Pathol (2011) 64:701–5. 10.1136/jcp.2011.090852
24.
Pignolo RJ Baujat G Brown MA De Cunto C Di Rocco M Hsiao EC et al Natural history of fibrodysplasia ossificans progressiva: cross-sectional analysis of annotated baseline phenotypes. Orphanet J Rare Dis (2019) 14:98. 10.1186/s13023-019-1068-7
25.
West RB Rubin BP Miller MA Subramanian S Kaygusuz G Montgomery K et al A landscape effect in tenosynovial giant-cell tumor from activation of CSF1 expression by a translocation in a minority of tumor cells. Proc Natl Acad Sci USA (2006) 103:690–5. 10.1073/pnas.0507321103
26.
Agaimy A Michal M Stoehr R Ferrazzi F Fabian P Michal M et al Recurrent novel HMGA2-NCOR2 fusions characterize a subset of keratin-positive giant cell-rich soft tissue tumors. Mod Pathol (2021) 34:1507–20. 10.1038/s41379-021-00789-8
27.
Panagopoulos I Andersen K Gorunova L Lund-Iversen M Lobmaier I Heim S . Recurrent fusion of the genes for high-Mobility group AT-hook 2 (HMGA2) and nuclear receptor Co-repressor 2 (NCOR2) in osteoclastic giant cell-rich tumors of bone. Cancer Genomics Proteomics (2022) 19:163–77. 10.21873/cgp.20312
28.
Vorontsov E Bozkurt A Casson A Shaikovski G Zelechowski M Severson K et al A foundation model for clinical-grade computational pathology and rare cancers detection. Nat Med (2024) 30:2924–35. 10.1038/s41591-024-03141-0
29.
Chen RJ Ding T Lu MY Williamson DFK Jaume G Song AH et al Towards a general-purpose foundation model for computational pathology. Nat Med (2024) 30:850–62. 10.1038/s41591-024-02857-3
30.
Xu H Usuyama N Bagga J Zhang S Rao R Naumann T et al A whole-slide foundation model for digital pathology from real-world data. Nature (2024) 630:181–8. 10.1038/s41586-024-07441-w
31.
Rau TT Cross W Lastra RR Lo RC-L Matoso A Herrington CS . Closing the loop - the role of pathologists in digital and computational pathology research. J Pathol Clin Res (2024) 10:e12366. 10.1002/2056-4538.12366
32.
WHO Classification of Tumours Editorial Board. Soft tissue and bone tumours. In: International agency for research on cancer. 5th ed. Lyon (France): WHO classification of tumours series (2020). Available online at: https://publications.iarc.fr/588 (Accessed April 7, 2025).
33.
WHO Classification of Tumours Editorial Board. Digestive system tumours. In: International agency for research on cancer. 5th ed. Lyon (France): WHO classification of tumours series (2019). Available online at: https://publications.iarc.fr/579 (Accessed April 7, 2025).
34.
WHO Classification of Tumours Editorial Board. Breast tumours. In: International agency for research on cancer. 5th ed. Lyon (France): WHO classification of tumours series (2019). Available online at: https://publications.iarc.fr/581 (Accessed April 7, 2025).
35.
WHO Classification of Tumours Editorial Board. Skin tumours. In: International agency for research on cancer. 5th ed. Lyon (France): WHO classification of tumours series (2023). Available online at: https://tumourclassification.iarc.who.int/chapters/64 (Accessed April 7, 2025).
36.
WHO Classification of Tumours Editorial Board. Head and neck tumours. In: International agency for research on cancer. 5th ed. Lyon (France): WHO classification of tumours series (2023). Available online at: https://publications.iarc.who.int/629 (Accessed April 7, 2025).
37.
WHO Classification of Tumours Editorial Board. Eye tumours. In: International agency for research on cancer. 5th ed. Lyon (France): WHO classification of tumours series (2023).
38.
WHO Classification of Tumours Editorial Board. Thoracic tumours. In: International agency for research on cancer. 5th ed. Lyon (France): WHO classification of tumours series (2021). Available online at: https://publications.iarc.fr/595 (Accessed April 7, 2025).
39.
WHO Classification of Tumours Editorial Board. Paediatric tumours. In: International agency for research on cancer. 5th ed.; vol. 7. Lyon (France): WHO classification of tumours series (2022). Available online at: https://publications.iarc.fr/608 (Accessed April 7, 2025).
40.
WHO Classification of Tumours Editorial Board. Urinary and Male genital tumours. In: International agency for research on cancer. 5th ed.Lyon (France): WHO classification of tumours series (2022). Available online at: https://publications.iarc.fr/610 (Accessed April 7, 2025).
41.
WHO Classification of Tumours Editorial Board. Haematolymphoid tumours. In: International agency for research on cancer. 5th ed. Lyon (France): WHO classification of tumours series (2024). Available online at: https://publications.iarc.who.int/637 (Accessed April 7, 2025).
42.
Zhu P Sun K Lao IW Yu L Bai Q Zhou X et al Expanding the spectrum of NUTM1-Rearranged sarcoma: a clinicopathologic and molecular genetic study of 8 cases. Am J Surg Pathol (2024) 48:930–41. 10.1097/PAS.0000000000002254
43.
Jakša R Stružinská I Kendall Bártů M Trča S Matěj R Dundr P . Clear cell stromal tumor of the lung with multinucleated giant cells: a report of a case with YAP1-TFE3 fusion. Diagn Pathol (2023) 18:9. 10.1186/s13000-023-01304-0
44.
Fritchie KJ Torres-Mora J Inwards C Thway K Vaiyapuri S Jackson R et al Xanthogranulomatous epithelial tumor: report of 6 cases of a novel, potentially deceptive lesion with a predilection for young women. Mod Pathol (2020) 33:1889–95. 10.1038/s41379-020-0562-8
45.
Yenwongfai LN Liu J Wang C Bocklage TJ . Extraskeletal osteosarcoma and its histological mimics. Hum Pathol Rep (2022) 28:300639. 10.1016/j.hpr.2022.300639
46.
Folpe AL Weiss SW . Ossifying fibromyxoid tumor of soft parts: a clinicopathologic study of 70 cases with emphasis on atypical and malignant variants. Am J Surg Pathol (2003) 27:421–31. 10.1097/00000478-200304000-00001
47.
Torres-Mora J Dry S Li X Binder S Amin M Folpe AL . Malignant melanotic schwannian tumor: a clinicopathologic, immunohistochemical, and gene expression profiling study of 40 cases, with a proposal for the reclassification of “melanotic schwannoma.”. Am J Surg Pathol (2014) 38:94–105. 10.1097/PAS.0b013e3182a0a150
48.
Murphey MD Gibson MS Jennings BT Crespo-Rodríguez AM Fanburg-Smith J Gajewski DA . From the archives of the AFIP: imaging of synovial sarcoma with radiologic-pathologic correlation. Radiographics (2006) 26:1543–65. 10.1148/rg.265065084
49.
Serinelli S Mookerjee GG Stock H De La Roza G Damron T Gitto L et al Low-grade fibromyxoid sarcoma with heterotopic bone formation: case report and review of the literature. Appl Immunohistochem and Mol Morphol (2022) 30:640–6. 10.1097/pai.0000000000001059
50.
Lu L Lao IW Liu X Yu L Wang J . Nodular fasciitis: a retrospective study of 272 cases from China with clinicopathologic and radiologic correlation. Ann Diagn Pathol (2015) 19:180–5. 10.1016/j.anndiagpath.2015.03.013
51.
Maqbool H Bashir S Hassan U Hussain M Mushtaq S Ishtiaq S . Angiomatoid fibrous histiocytoma: a tumor with uncertain behavior and various clinicopathological presentations. Cureus (2022) 14:e28985. 10.7759/cureus.28985
52.
Ushijima M Hashimoto H Tsuneyoshi M Enjoji M . Giant cell tumor of the tendon sheath (nodular tenosynovitis). A study of 207 cases to compare the large joint group with the common digit group. Cancer (1986) 57:875–84. 10.1002/1097-0142(19860215)57:4<875::aid-cncr2820570432>3.0.co;2-y
53.
Somerhausen NS Fletcher CD . Diffuse-type giant cell tumor: clinicopathologic and immunohistochemical analysis of 50 cases with extraarticular disease. Am J Surg Pathol (2000) 24:479–92. 10.1097/00000478-200004000-00002
54.
Moosavi C Jha P Fanburg-Smith JC . An update on plexiform fibrohistiocytic tumor and addition of 66 new cases from the armed forces institute of pathology, in honor of franz M. Enzinger, MD. Ann Diagn Pathol (2007) 11:313–9. 10.1016/j.anndiagpath.2007.01.003
55.
Oliveira AM Dei Tos AP Fletcher CD Nascimento AG . Primary giant cell tumor of soft tissues: a study of 22 cases. Am J Surg Pathol (2000) 24:248–56. 10.1097/00000478-200002000-00011
56.
Montgomery EA Meis JM . Nodular fasciitis. Its morphologic spectrum and immunohistochemical profile. Am J Surg Pathol (1991) 15:942–8. 10.1097/00000478-199110000-00004
57.
Cancer Genome Atlas Research NetworkCancer Genome Atlas Research Network. Electronic address: elizabeth.demicco@sinaihealthsystem.ca, cancer genome atlas research network. Comprehensive and integrated genomic characterization of adult soft tissue sarcomas. Cell (2017) 171:950–65.e28. 10.1016/j.cell.2017.10.014
58.
Green C Spagnolo DV Robbins PD Fermoyle S Wong DD . Clear cell sarcoma of the gastrointestinal tract and malignant gastrointestinal neuroectodermal tumour: distinct or related entities? A review. Pathology (2018) 50:490–8. 10.1016/j.pathol.2018.05.001
59.
Miettinen M Lasota J . Gastrointestinal stromal tumors. Gastroenterol Clin North Am (2013) 42:399–415. 10.1016/j.gtc.2013.01.001
60.
Simonet WS Lacey DL Dunstan CR Kelley M Chang MS Lüthy R et al Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell (1997) 89:309–19. 10.1016/s0092-8674(00)80209-3
61.
Abrahamsen B Teng AYT . Technology evaluation: Denosumab, amgen. Curr Opin Mol Ther (2005) 7:604–10.
62.
Lacey DL Timms E Tan HL Kelley MJ Dunstan CR Burgess T et al Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell (1998) 93:165–76. 10.1016/s0092-8674(00)81569-x
63.
Behjati S Tarpey PS Presneau N Scheipl S Pillay N Van Loo P et al Distinct H3F3A and H3F3B driver mutations define chondroblastoma and giant cell tumor of bone. Nat Genet (2013) 45:1479–82. 10.1038/ng.2814
64.
Divisato G Formicola D Esposito T Merlotti D Pazzaglia L Del Fattore A et al ZNF687 mutations in severe paget disease of bone associated with giant cell tumor. Am J Hum Genet (2016) 98:275–86. 10.1016/j.ajhg.2015.12.016
65.
Wei Z Li S Tao X Zhu G Sun Z Wei Z et al Mutations in profilin 1 cause early-onset paget’s disease of bone with giant cell tumors. J Bone Miner Res (2021) 36:1088–103. 10.1002/jbmr.4275
66.
Gennari L Rendina D Merlotti D Cavati G Mingiano C Cosso R et al Update on the pathogenesis and genetics of Paget’s disease of bone. Front Cell Dev Biol (2022) 10:932065. 10.3389/fcell.2022.932065
Summary
Keywords
digital pathology, osteoclast, artificial intelligence, mineralisation, soft tissue tumour
Citation
Al Khader A, Seghetti C, Oumlil F, Tollit A, Tirabosco R, Amary F, O’Donnell P and Flanagan AM (2025) The value of morphology: osteoclast-like cells in soft tissue tumours. Pathol. Oncol. Res. 31:1612175. doi: 10.3389/pore.2025.1612175
Received
14 May 2025
Accepted
22 August 2025
Published
12 September 2025
Volume
31 - 2025
Edited by
Zsolt Orosz, Nuffield Orthopaedic Centre, United Kingdom
Updates
Copyright
© 2025 Al Khader, Seghetti, Oumlil, Tollit, Tirabosco, Amary, O’Donnell and Flanagan.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adrienne M. Flanagan, a.flanagan@ucl.ac.uk
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.