Abstract
Tumor-to-tumor metastasis is a rare phenomenon. Although renal cell carcinoma is the most common recipient tumor, metastatic lobular breast carcinoma to clear cell renal cell carcinoma is even rarer, with only one case reported to date. We present a 66-year-old female patient with an invasive lobular carcinoma history who was admitted to the hospital with a right renal mass. The patient received partial nephrectomy. The final established diagnosis is lobular breast carcinoma metastasizing to clear cell renal cell carcinoma (ccRCC). Thus, although rare, the simultaneous or consecutive find of a renal mass in follow-up should be carefully evaluated, especially in high-risk patients, including women with an advanced breast cancer history, as in this scenario.
Background
Tumor-to-tumor metastasis (TTM), usually defined as one malignant tumor metastasizing to another unrelated primary tumor, is a rare phenomenon. It was first described in 1902 by Berent, and no more than 200 cases have been reported in the literature within the last few decades [1–3]. The most common malignant recipient tumor was renal cell carcinoma (RCC, 38.8%), and the most common donor tumor was lung cancer (55.8%) [4]. To the best of our knowledge, no more than 10 cases of breast cancer metastasis to an RCC have been reported, among which only one case documented lobular breast carcinoma metastasis [5].
We reported a rare case of primary advanced stage invasive lobular carcinoma metastasis to renal clear cell carcinoma after surgery followed by adjuvant hormonal therapy, and a detailed pathological examination was performed.
Case presentation
A 66-year-old woman was admitted to the hospital with a past medical history of advanced invasive lobular carcinoma of the left breast diagnosed 3 years prior. In 2018, the patient was initially diagnosed with invasive lobular carcinoma via biopsy (ER 90%+; PR -; HER2 2+; FISH test: HER2-negative). Then neoadjuvant chemotherapy was administered, followed by modified radical mastectomy. Lymph node metastases were found (29/29). After surgery, several cycles of radiotherapy/adjuvant therapy were administered. Computerized tomography (CT) scan was performed regularly as part of her follow-up. At this time, CT examination revealed a dense well-circumscribed solid nodule, measuring 2.1 cm × 1.9 cm. For further examination, the patient underwent enhanced magnetic resonance imaging (MRI). A 2.4 cm × 2.3 cm × 1.9 cm lesion was observed in the middle of the right kidney, displaying varying degrees and extents of T2 hyperintensity. The patient underwent partial nephrectomy.
Grossly, the tumor measured 2.0 cm in greatest dimension and had a yellowish and brown-tan appearance. Microscopic examination revealed two distinct but intermingled populations of cells. The neoplastic cells of the first lesion demonstrated typical clear cell renal cell carcinoma (ccRCC) pattern, showing clear cytoplasm with round nuclei and inconspicuous nucleoli (WHO/ISUP grade 1) (Figure 1). Immunohistochemical stains confirmed this neoplasm as ccRCC: it was positive for CA IX, CD10, PAX8, PAX2, and Vimentin; negative for CD117, CK7 and breast carcinoma markers (Figure 2).
FIGURE 1
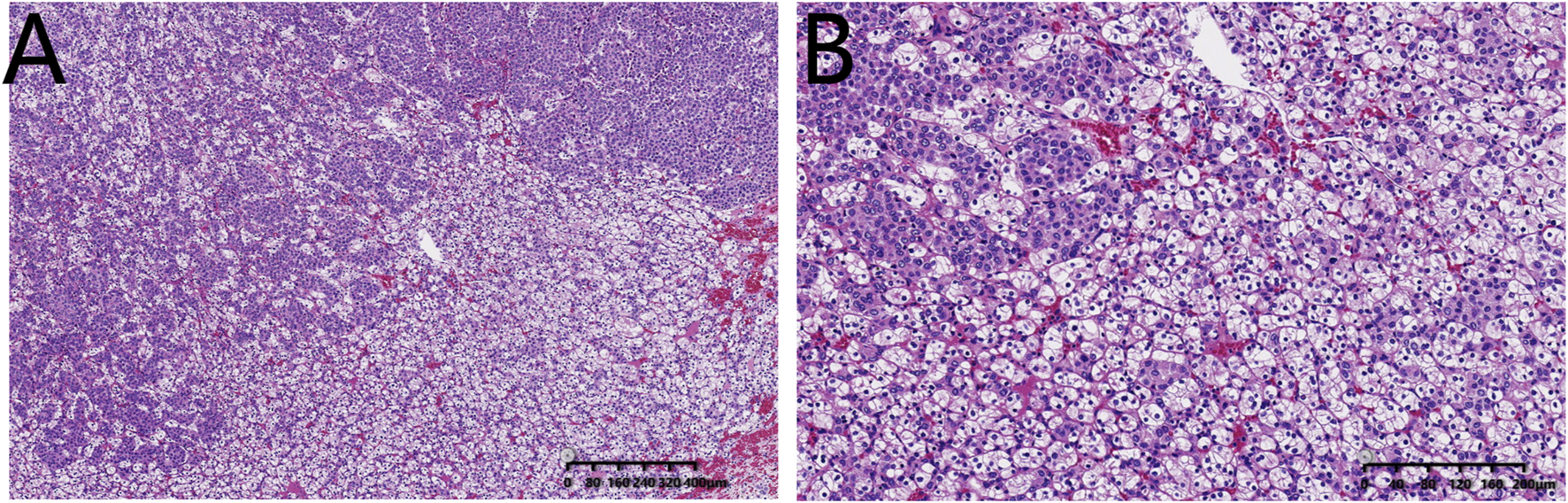
Hematoxylin and eosin stained (H&E) sections of the clear renal cell carcinoma with metastatic infiltrating lobular breast carcinoma. Clusters of breast cancer cells are embedded within ccRCC [(A): bar = 400 μm; (B): bar = 200 μm].
FIGURE 2
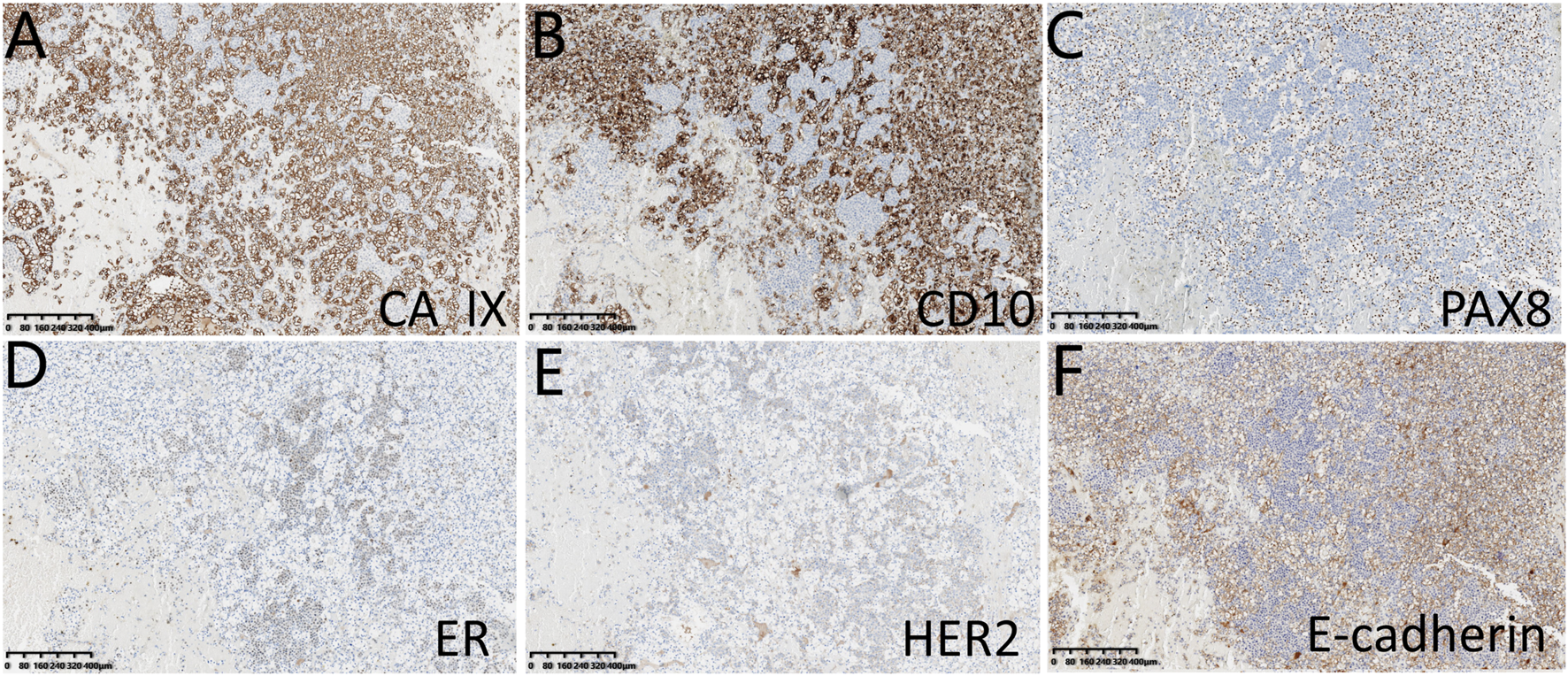
Immunohistochemical staining of panel for ccRCC and panel for lobular breast carcinoma. (A–C) representative ccRCC markers: CA IX, CD10, and PAX8; (D–F) representative lobular breast carcinoma markers: ER, HER2 and E-cadherin. Bar = 400 μm.
Metastatic invasive lobular carcinoma of the breast was observed within the ccRCC (Figure 1), forming nests or clusters of small cells, which exhibited diffuse growth pattern that invaded a “pool” of clear cells. The neoplastic cells exhibited basophilic cytoplasm, with round or ovoid nuclei exhibiting moderate nuclear pleomorphism. Lymphovascular invasion and nerve invasion were also detected. Several breast lobular carcinoma markers were positive: ER (80%+), HER2 (1+) (Figure 2), and GCDFP15(1+) (Figure 3) while renal cell carcinoma markers were negative, indicating the exclusion of ccRCC. Loss of expression of E-cadherin on immunohistochemical staining further confirmed the tumor phenotype.
FIGURE 3
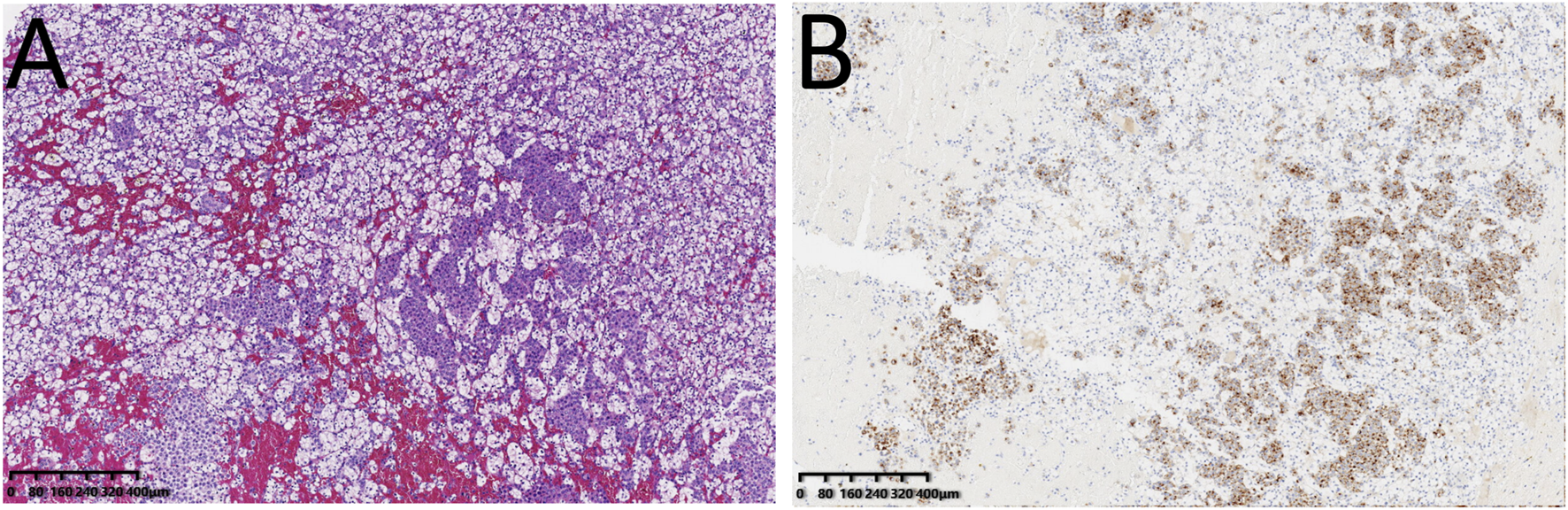
Immunohistochemical staining of GCDFP15 (B) with corresponding H&E section (A), confirming lesions originated of breast. Bar = 400 μm.
No further treatment was administered after surgery in our case. The recent follow-up indicates the patient is still alive, which is 57 months after diagnosis of her primary disease and 7 months following the development of breast secondaries.
Discussion and conclusion
The presence of two synchronous cancers in one patient remains fairly uncommon. The criteria for diagnosis of tumor-to-tumor metastasis was originally described in 1968 [6] and was further modified, especially addressing the importance of the metastatic tumor epicenter considering true tumor-in-tumor [7, 8]. First, the recipient tumor and the donor tumor must be two different tumors, and both must be true neoplasms. Second, if tumors metastasize to the lymphatic system with a primary lymphatic malignancy, then in such situations it cannot be defined as tumor-to-tumor metastasis. Third, the evidence of the primary carcinoma must be solid. Fourth, the primary and metastatic tumors must be compatible, as proven by morphology and immunohistochemical staining. Last, the metastatic lesions must be at least partially enclosed by a rim of histologically distinct host tumor tissue. Examining all the above criteria, the case we reported can be diagnosed as a true tumor-to-tumor metastasis.
Prior to our case, very few reports of breast cancer metastasizing to renal cell carcinoma have been documented. In 2005, one case reported that a 62-year-old white woman with an infiltrating ductal carcinoma history developed clear cell renal cell carcinoma (RCC) (stage T1aN0M0), which involved multiple foci of metastatic breast carcinoma 2 years after mastectomy [2]. Another case report described a 43-year-old female diagnosed with an invasive duct carcinoma (T2N0M0), who received a modified radical mastectomy in 2010. Four years after mastectomy, ccRCC with a small distinct focus of breast carcinoma was detected. Considering the imaging, medical history, and histology, a final diagnosis of duct breast carcinoma metastasizing to RCC was established [9]. During the process of establishing the final diagnosis, in addition to imaging and medical history, unique morphology of breast cancer, which is usually significantly different from RCC, is the key for right diagnosis. A panel of immunohistochemical staining markers including RCC markers CA IX, CD10, PAX8, PAX2, CD117, CK7 and breast cancer markers ER, PR, GCDFP15 would facilitate histopathological differential diagnosis.
Metastatic lobular breast carcinoma to clear cell renal cell carcinoma is even rarer. To the best of our knowledge, in all the English literature we searched, only one similar case was published recently [5]. In that case, a 57-year-old woman with a past medical history of stage IIA (pT2 N0 M0) multifocal infiltrating lobular carcinoma was diagnosed with metastatic infiltrating lobular carcinoma involving clear cell renal cell carcinoma 11 years after the initial diagnosis. The patient remained on fulvestrant and Palbociclib and the disease was stable.
Although still not clear, several proposed mechanisms may partially explain the tumor-to-tumor metastasis. It is rare that breast cancer metastasizes to the kidneys, but RCC is still found in up to 65% of tumor-to-tumor metastasis cases. Several theories contribute to such predisposition: 1) high content of glycogen and lipid rich cells; 2) lower immune competence of RCC and 3) a well-preserved stroma [2, 10, 11]. All these factors are consistent with the “seed and soil” theory first described by Sir Steven Paget in 1889 and the “mechanical” theory suggested by Ewing in 1928 [12, 13]. In our case, massive lymph node metastases also suggest more chances of “seeding.”
In conclusion, although a rare event, tumor-to-tumor metastasis should be considered with careful assessment and adequate histology examination, especially in advanced stage cancer. Supporting evidence of sufficient immunohistochemical staining will also facilitate diagnosis and differential diagnosis.
Statements
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LZ, PY, and CG wrote the main manuscript text and prepared Figures 1–3. QC, JM, CG, and JY performed histology examination and diagnosis. All authors contributed to the article and approved the submitted version.
Funding
This project was supported by the National Anti-Tumor Drug Surveillance System of National Cancer Center (No. DSS-YSF2022-08).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Richardson JF Katayama I . Neoplasm to neoplasm metastasis. An acidophil adenoma harbouring metastatic carcinoma: A case report. Arch Pathol (1971) 91:135–9.
2.
Möller MG Gribbin T Ebrom S Padula G Fitzgerald TL . Breast cancer metastatic to renal cell carcinoma. Surgery (2006) 139:577–9. 10.1016/j.surg.2005.10.016
3.
Ricketts R Tamboli P Czerniak B Guo CC . Tumor-to-Tumor metastasis: Report of 2 cases of metastatic carcinoma to angiomyolipoma of the kidney. Arch Pathol Lab Med (2008) 132:1016–20. 10.1043/1543-2165(2008)132[1016:TMROCO]2.0.CO;2
4.
Chen TD Lee LY . A case of renal cell carcinoma metastasizing to invasive ductal breast carcinoma. J Formos Med Assoc (2014) 113:133–6. 10.1016/j.jfma.2012.07.022
5.
Ashman D Quiroga-Garza G Lee D . Rare presentation of metastatic lobular breast carcinoma involving clear cell renal cell carcinoma. Case Rep Oncol Med (2020) 2020:5315178. 10.1155/2020/5315178
6.
Campbell LV Jr Gilbert E Chamberlain CR Jr Watne AL . Metastases of cancer to cancer. Cancer (1968) 22:635–43. 10.1002/1097-0142(196809)22:3<635::aid-cncr2820220320>3.0.co;2-o
7.
Pamphlett R . Carcinoma metastasis to meningioma. J Neurol Neurosurg Psychiatry (1984) 47:561–3. 10.1136/jnnp.47.5.561
8.
Takei H Powell SZ . Tumor-to-tumor metastasis to the central nervous system. Neuropathology (2009) 29:303–8. 10.1111/j.1440-1789.2008.00952.x
9.
Huo Z Gao Y Yu Z Zuo W Zhang Y . Metastasis of breast cancer to renal cancer: Report of a rare case. Int J Clin Exp Pathol (2015) 8:15417–21. eCollection 2015.
10.
Sella A Ro JY . Renal cell cancer: Best recipient of tumor-to-tumor metastasis. Urology (1987) 30:35–8. 10.1016/0090-4295(87)90568-1
11.
Beisland C Talleraas O Bakke A Norstein J . Multiple primary malignancies in patients with renal cell carcinoma: A national population-based cohort study. BJU Int (2006) 97:698–702. 10.1111/j.1464-410X.2006.06004.x
12.
Granville LA Ostrowski ML Truong LD Shen S . Pathologic quiz case: Unusual morphology in an otherwise classic renal cell carcinoma. In: Tumor-to-tumor metastasis: Pulmonary adenocarcinoma metastatic to clear cell renal cell carcinoma (2005).
13.
Fidler IJ Poste G . The “seed and soil” hypothesis revisited. Lancet Oncol (2008) 9:808. 10.1016/S1470-2045(08)70201-8
Summary
Keywords
breast cancer, clear cell renal cell carcinoma, tumor-to-tumor metastasis, rare case, metastatic lobular breast carcinoma
Citation
Zhang L, Yuan P, Cao Q, Mu J, Ying J and Guo C (2023) RETRACTED: Case report: A rare case of tumor-to-tumor metastasis: metastatic lobular breast carcinoma to clear cell renal cell carcinoma. Pathol. Oncol. Res. 29:1611204. doi: 10.3389/pore.2023.1611204
Received
26 March 2023
Accepted
31 May 2023
Published
12 June 2023
Volume
29 - 2023
Edited by
Gabor Cserni, University of Szeged, Hungary
Updates
Copyright
© 2023 Zhang, Yuan, Cao, Mu, Ying and Guo.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Changyuan Guo, guocycicams@sina.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.